32: Proximal Hypospadias
阅读本章大约需要 26 分钟。
Introduction
Hypospadias is defined as an opening of the urethral meatus on the ventral aspect of the penile shaft proximal to the tip of the glans penis. As mentioned in the previous chapter, hypospadias is classified according to the location of the urethral meatus as distal, middle, and proximal. The posterior (severe) variety, which accounts for 20% of the cases, extends through the proximal third of the penile shaft to the perineum. It may further be sub-classified as posterior penile (at the base of the shaft), penoscrotal (at the base of the shaft in front of the scrotum), scrotal (on the scrotum or in between the genital swellings) or the most severe variety, the perineal (behind the scrotum and behind the genital swellings, Figure 1).1 Although the classification of hypospadias, to distal, mid shaft and proximal has been historically based on meatal location preoperatively, the correct classification is best done at the time of surgery, since meatal location may change based on hypoplastic urethral more proximally. The severe hypospadias is often associated with ventral curvature of the penis known as chordee, a “hooded” or incomplete prepuce, and an abortive corpora spongiosum. Hypospadiology, a term coined by John W. Duckett, Jr., is the study of all aspects of this condition and encompasses a continuously evolving and expanding discipline.2 The incidence of hypospadias is about 1:200–300 live births in the US.3,4 The recent increase in incidence can be attributed to prematurity, small-for-gestational age infants, low birth weight and maternal age of 35 years or older.1
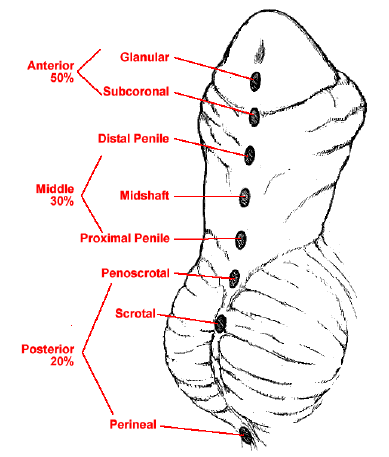
Figure 1 Spectrum of hypospadias presentations.
Embryology
The male external genitalia progressively develops recognisable characteristics by the 3rd month of gestation. Normally, the urogenital sinus opening extends to the ventral aspect of the genital tubercle as the urethral groove. The primitive urogenital orifice and the urethral groove are bound on either side by the urethral folds.5 The genital tubercle becomes elongated to form the phallus, and the urethral folds start to fuse from the urogenital orifice towards the tip of the phallus, which results in the formation of the penile urethra by the end of the 14th week. The corpora cavernosa appear as paired mesenchymal columns within the shaft of the penis in the 7th week. The corpora spongiosa results from the differentiation of the mesenchymal masses around the penile urethra.5 In cases of proximal hypospadias, it is believed that there is failure of these urethral folds to fuse. Due to the arrest in the tubularisation, there is differential growth of the penis on the ventral as compared to the dorsal aspect.
An understanding of the anatomy of the penis will greatly aid in understanding the repair of hypospadias (Figure 2).
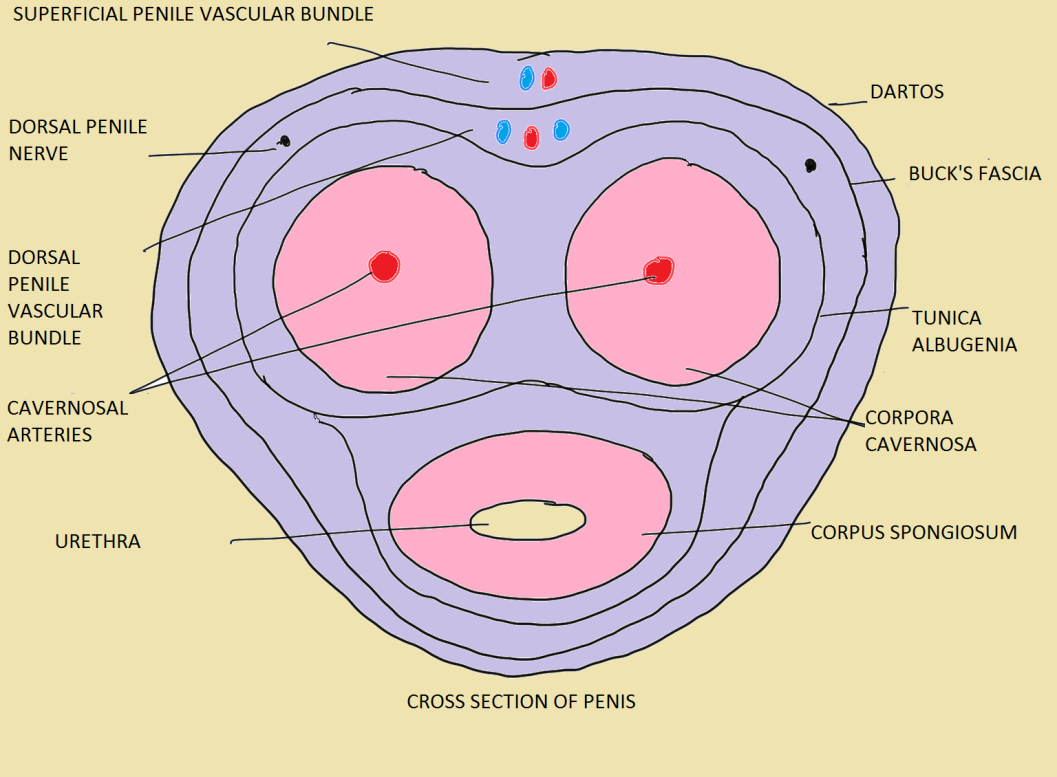 Figure 2 The layers of the penis in a normal adult.6
Figure 2 The layers of the penis in a normal adult.6
Severe Hypospadias and Other Associated Genitourinary Conditions
Due to common embryopathy, proximal hypospadias is more often associated with other congenital conditions namely cryptorchoidism in 10% of cases,7 inguinal hernia in up to 32% of boys,8 disorders of sexual development in up to 27.3%9 and prostatic utricle.
In the presence of severe hypospadias and a nonpalpable testes, DSD must be ruled out.10 In these cases, obtaining a karyotype is a must. Scrotal hypospadias alone should raise suspicion about disorder of sex development, more so when it is associated with bilateral cryporchoidism.11 Ambiguous genitalia is suspected in patients of hypospadias with impalpable gonads; hypospadias with micropenis and either one or no palpable gonads; new born with female external genitalia and a gonadal mass in the labia or labial fusion and/or clitoral enlargement.12
Evaluation
Table 1 Points to note while evaluating a case of hypospadias.6
| History | Additional History | Examination | Additional examination |
|---|---|---|---|
| age, reared as male | h/o voice change, breast development | stretched phallic length | habitus (masculine or feminine) |
| h/o passing urine from under surface of penis | h/o maternal intake of hormones during pregnancy | chordee (absent/mild <30˚/severe >30˚) | breast development (Tanner’s staging) |
| ventral curvature of penis | family history of hypospadias | meatus (stenotic/ not stenotic) | axillary Hair (present or absent, development of male or female type) |
| urinary stream deviated from midline or narrow | h/o repeated fetal loss or acute illness and vomiting in neonatal period | meatal location (glandular/coronal/distal penile/mid penile/proximal penile/penoscrotal/scrotal) | pubic hair (present or absent, development of male or female type) |
| h/o genital surgery | glans (rounded/conical) | ambiguity of external genitalia (Prader’s staging in a case of DSD) | |
| undescended testis | urethral groove (shallow/deep) | ||
| h/o erections and curvature in an older adolescent child | urethral plate (wide/narrow/scarred/supple) | ||
| prepuce (dorsal hooded/adequate for reconstruction/absent) | |||
| testes location | |||
| testes size | |||
| scrotum (well developed/penoscrotal transposition/hypoplastic/penoscrotal webbing) |
In addition, the GMS (Glans, Meatus, and Shaft) score appears to correlate with the risk of a surgical complications. The GMS score is based on the glans size/urethral plate quality, location of meatus, and degree of chordee. Arlen et al demonstrated a statistically significant increase in the likelihood of any postoperative complication with every unit increase in total GMS score Table 2.13 In their study, 262 boys (mean age 12.3 ± 13.7 months) underwent primary hypospadias repair had a mean GMS score of 7 ± 2.5 (G 2.1 ± 0.9, M 2.4 ± 1, S 2.4 ± 1) and a mean clinical follow-up of 17.7 ± 9.3 months. They found 37 boys developed 45 complications. A significant relationship between the total GMS score and the presence of any complication (p < 0.001) was observed; for every unit increase in GMS score the odds of any postoperative complication increased 1.44 times (95% CI, 1.24–1.68).13 The development of a urethrocutaneuous fistula was observed in 21 of 239 (8.8%) of single-stage repairs and was the most common complication. Those with mild (GMS 3–6), moderate (GMS 7–9) and severe (GMS 10–12) hypospadias had a 2.4% fistula, 11.1%, and 22.6% (p < 0.001) fistula rate respectively. Also, the degree of chordee was observed to be an independent predictor of fistula on multivariate analysis. They found that patients with greater than 60° ventral curvature were 27 times more likely to develop a fistula than patients who had no curvature (95% CI, 3.2–229).13
Table 2 The GMS score.13
| Glans (G) Score | Meatus (M) Score | Shaft (S) Score |
|---|---|---|
| 1. Glans good size; healthy urethral plate, deeply grooved | 1. Glanular | 1. No chordee |
| 2. Glans adequate size; adequate urethral plate, grooved | 2. Coronal sulcus | 2. Mild (< 30°) chordee |
| 3. Glans small in size; urethral plate narrow, some fibrosis or flat | 3. Mid or distal shaft | 3. Moderate (30–60°) chordee |
| 4. Glans very small; urethral plate indistinct, very narrow or flat | 4. Proximal shaft, penoscrotal | 4. Severe (> 60°) chordee |
The assessment of the urethral plate is also important as a narrow urethral plate portends poorer prognosis (Figure 3). The two predominant factors that guide our decision on how to repair a proximal hypospadias are the quality of the urethral plate, and perhaps more importantly, the degree of ventral curvature present
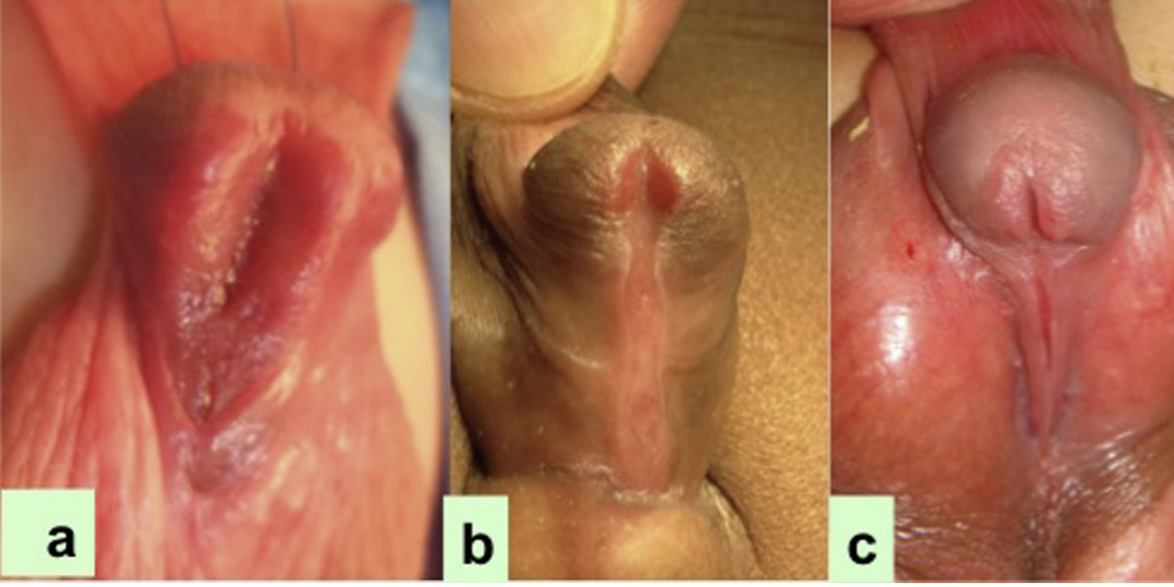
Figure 3 The width of the urethral plate decreases from a to c in the patients of proximal hypospadias.14
Investigations
Imaging
- The ultrasound should be done in cases of proximal hypospadias to rule out associated renal anomalies although such anomalies are extremely rare.12 If there is a history of recurrent urinary tract infection, a Micturating cystourethrography should be performed. Also, in cases of true ambiguous genitalia, MCU can help to assess the presence of müllerian duct remnants. These patients are usually asymptomatic and do not require routine surgical resection of the remnants. Occasionally, resection of the utricle may be necessary because of recurrent urinary tract infection, urinary dribbling or stone formation.12 While operating in patients with proximal hypospadias, the prostatic utricle might sometimes prevent placement of the catheter into the bladder with the catheter preferentially lodging in the utricle itself. This can be taken care of by using any of the following methods i) the double catheter method in which the first catheter inadvertently enters in the prostatic utricle, then a smaller French catheter is inserted through the urethral meatus and that invariably enters into the urethra; ii) the Clutton sound for guiding the urethral catheter; iii) in difficult cases, cystoscopy aided soft guide wire can be first passed into the bladder and then an open ended catheter can be advanced over the wire to reach the bladder.15
Karyotyping
The AUA cryptorchidism guideline recommends that all boys with unilateral or bilateral undescended testes and severe proximal hypospadias must undergo additional testing to rule out a disorder of sexual differentiation (DSD), which occurs much more frequently in these settings .9,10 Guidelines introduced in 2006 included severe hypospadias as a form of 46,XY DSD.16 The concern for DSD is particularly high in a boy with hypospadias and a nonpalpable testis. Kaefer et al.10 examined 79 patients with a history of hypospadias and cryptorchidism. Those with a nonpalpable testis(es), either unilateral or bilateral, had a threefold increased risk of having an underlying DSD diagnosis identified (approximately 50% vs. 15%). There was a significantly increased risk of DSD with proximal hypospadias compared with distal hypospadias (64% vs. 7%) .10 A normal 46, XY karyotype may be misleading, particularly in boys with the most severe variants. The authors also prefer investigating such patients with severe hypospadias and UDT with Karyotyping.
Preoperative Androgen
The preoperative use of DHT, or testosterone can be either by local application, or more frequently by intramuscular injection, can lead to an increase in penile length and width, and can cause an increase in glans size. In patients with micropenis, the testosterone has shown to be beneficial in stimulating the growth of the penis. The protocol of application may vary in different institutes. Local application of 2% testosterone propionate cream to the penis three times daily for 3 weeks is recommended.12 This route of testosterone administration is easy to apply, and shows good response. However, the response is variable depending upon the compliance of daily application and the amount of cream applied. Excess amount may lead to systemic absorption, deepening of voice and change in behaviour of boys in extreme cases. The application should be stopped at least a 3 week before the date of surgery. The intramuscular testosterone, 2mg/kg/dose total of three doses at 3 weeks interval, the last dose given at least 2 weeks prior to the date of surgery, is a more reliable route of administration.
Consent for Surgery
A fully informed written consent must be obtained after giving appropriate, enough, timely information about the planned procedure and the possible alternate procedures which would best apply to the individual case. Many times, the procedure may change depending upon the examination under anaesthesia and hence, the possibility of various surgical options should be informed to parent beforehand. A clear picture of the outcome, cosmetic results and possible complications (fistula formation, stricture or dehiscence) must be provided. In cases of proximal hypospadias, parents must understand that their child most probably requires a multistage repair. Thus, preparation of the family and patient for the proper procedure, accurate anatomic assessment, and an honest discussion about surgical outcomes and potential complications is necessary.7
Surgical Timing
The timing of the primary elective repair is recommended to occur between the ages of 6 and 12 months by the American Academy of Pediatrics [AAP]7,17 based on studies that highlight the balance between the potential adverse psychological effects of surgery, the anesthetic risk to the child, the degree of penile development that will facilitate a successful repair, and wound healing differences as boys age.18 Belman et al showed that boys undergoing repair before 12 months of age, experienced less anxiety and had improved psychosexual outcomes compared with boys undergoing repair at older ages.19
Objectives of Reconstruction
- To enable voiding with normal velocity and laminar flow,
- To obtain satisfactory sexual function with a straight penis, and
- Achievement of a slit-like meatus with a well approximated glans, from a cosmetic stand point.20
Stages of Reconstruction
- Correction of ventral curvature
- Urethroplasty
- Glansplasty
- Skin coverage
Surgical Repair Techniques
In proximal hypospadias, these are most often achieved by staged repair. There are two schools of thought regarding proximal hypospadias repair:
- use of flaps
- staged graft procedures
These are dependent on the correction of ventral curvature. On rare occasions, after skin degloving there is no further ventral chordee, and either Tubularised incised Plate (TIP) repair or Onlay island flap is used for urethroplasty, although the long TIP repair is less in favour, because of long-term complications. If there is left over chordee, some surgeons prefer the staged repair wherein, after dividing the urethral plate, they place a preputial graft, and if not available, a buccal mucosal graft (BMG) in the first stage and then tabularize the graft at the second stage. If after skin degloving there is still ventral curvature above 30 degrees, then correction of the chordee, either by Tunica vaginalis flap (TVF), or Tunica vaginalis graft (TVG), or SIS, or dermal, or by multiple transverse corprotomies as explained by Snodgrass21 is used in the first stage. Then urethroplasty is done in the second or third stage of repair, based on the technique for correcting the ventral chordee.
In short, if, after the skin degloving, there is Chordee< 30, then there are 2 options: TIP repair (not preferred by most surgeons), and the dorsal only flap.
If the chordee is > 30˚, then the Urethral plate (UP) is divided. Now if after division there is no chordee, we can use dorsal preputial flap as inlay or as tabularized (after Duckett) or we can use preputial or BMG graft.
Correction of Penile Ventral Curvature
Chordee Overview
The chordee correction is the most important initial step in the repair of proximal hypospadias, whether staged or single stage. In the first stage after degloving the penile skin, the degree of penile curvature is evaluated by artificial erection test. If the chordee is above 30 degrees, measured by ruler or goniometer (Figure 4), then next step would be to divide the urethral plate, which is mostly done at the distal end near the glans level. In this stage the ventral curvature is corrected, penoscrotal transposition is repaired, penile shaft skin is degloved and the urethral plate is divided to correct the curvature.
Moscardi et al.22 pointed out that a high percentage of penile curvatures were resolved just by degloving the penis, the shortened ventral skin, and fibrotic ventral dartos. Braga et al.23 reviewed the resolution rate of the penile curvature after the dissection of the skin and the dartos fascia in 137 patients with hypospadias7 where 9 had mild (<30°), 44 moderate (30–45°), and 85 had severe curvature (>45°). The complete resolution rate of the curvature, after degloving the penis was 70% in the mild, 30% in the moderate, and 2.4% in the severe curvature group.23
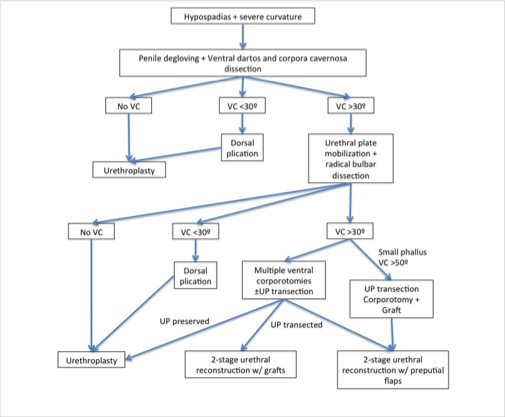
Figure 4 Management in patients with proximal penile hypospadias and chordee.22
Measurement of Degree of Chordee
The straightening of the penile shaft is measured using the test for artificial erection, i.e., Gittes and McLaughlin technique.24 In this test, saline is injected through a fine needle (25–27 gauge) into the lateral aspect of the corpora cavernosa or into the glans with a tourniquet at the base of the penis (Figure 5).
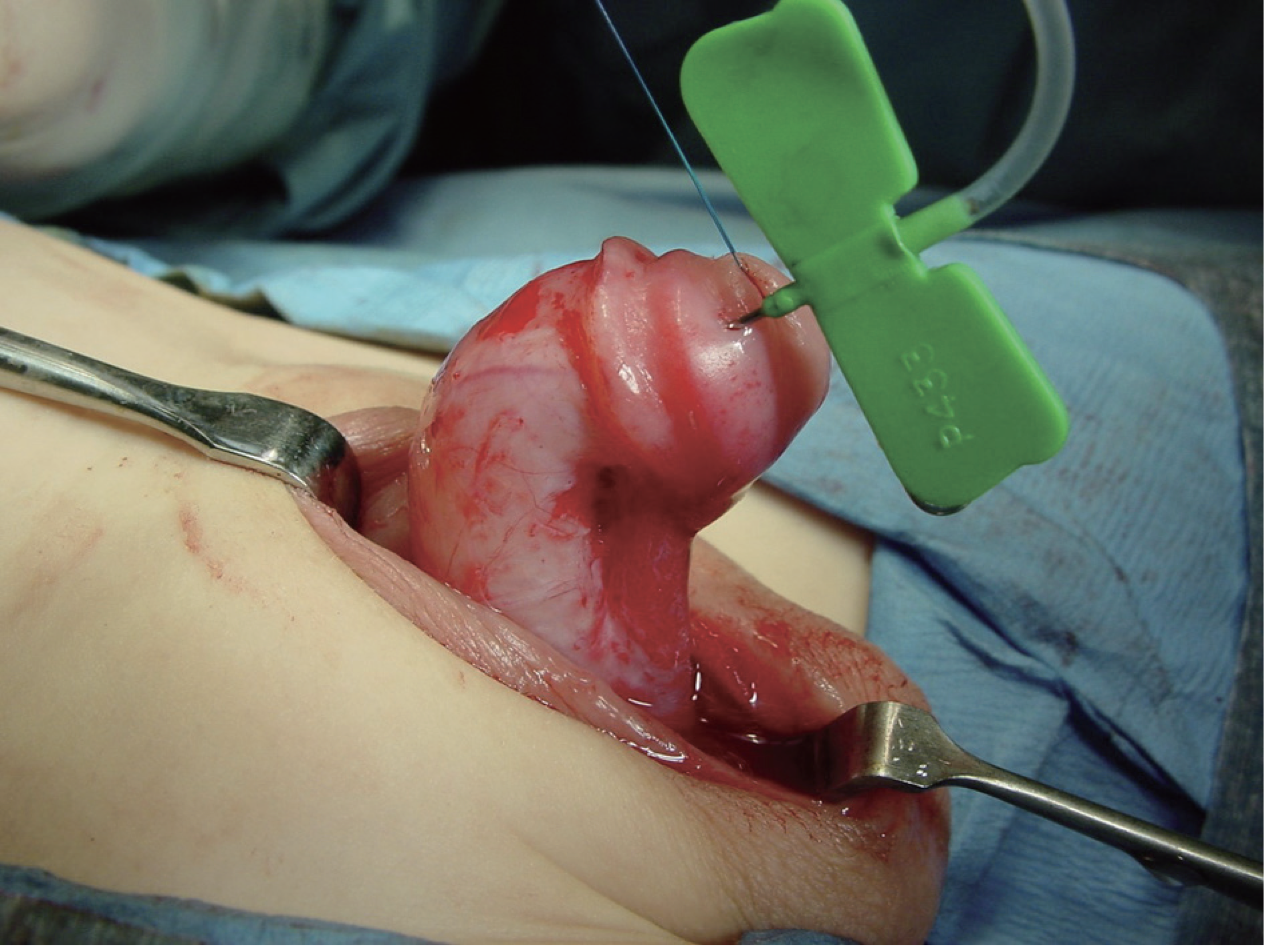
Figure 5 Measurement of degree of penile curvature intra-operatively.
However, in a high percentage of proximal hypospadias, after degloving, if an artificial erection shows more than 30 degrees of chordee, then the UP is divided at the distal end near the glans, and the proximal urethra is dissected to make the penis straight, improve the penile length and avoid retraction by the short and fibrotic urethral plate.22 The penile elongation techniques include execution of multiple transverse incisions on the ventral aspect of the tunica albuginea or, performing a single transverse incision and applying a graft or flap of tunica vaginalis, SIS graft, or dermis (Figure 6).

Figure 6 Correction of penile curvature by corporotomy and using SIS graft to cover the raw area.
Residual Chordee After Up Incision
In those cases where chordee still persists on the artificial erection test, after dividing the UP, there are two ways to deal with residual chordee, corporotomies i.e., making 3 transverse incisions ventrally, not very deep, without coverage by any graft, or the other way, that the authors also use, is to make one big transverse incision and then cover it by either dermal graft, SIS, TVG or TV FLAP (Figure 7).21
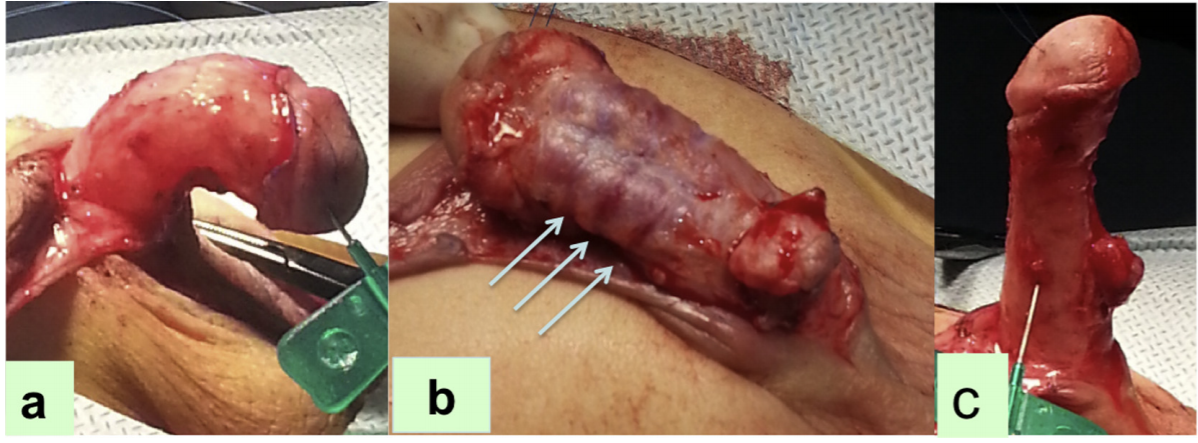
Figure 7 (a) The artificial erection test demonstrating degree of chordee, (b) Multiple transverse corporotomies, (c) Straightening of the penile curvature on repeated testing. [From: An alternative for ventral lengthening in children with severe penile curvature that allows graft coverage during staged hypospadias repair. Bruno Leslie, Bryce Weber, Rodrigo Romao, Walid Farhat, Darius Bagli, Armando Lorenzo, Joao Pippi Salle. J Urol Vol 221, Pg 11, 2011]
In the first technique, three transverse corporotomies are performed ventrally, first at the point of maximal curvature from 4 o’clock to 8 o’clock, and two more 5 mm proximal and 5 mm distal to the first, through the tunica albuginea till the erectile tissue is visible, and the test is then repeated. These corporotomies may be covered using the native proximal urethra, after proximal dissection, or covered by preputial graft or BMG.21,25
Snodgrass performed a study on 43 boys with proximal hypospadias and ventral curvature 30 degrees or greater after degloving underwent transection of the urethral plate. Those patients with persistent ventral curvature 30 degrees or greater also underwent 3 ventral corporotomies without corporal grafting for straightening. Staged graft urethroplasty was performed using prepuce, or labial mucosa.21,25,26 They found that the mean ventral curvature was 70 degrees, and corporotomy was performed in 65% of them and the preputial grafts were used in 88%; the rest of the patients, the corporotomy was covered by dermal grafts. None of these patients were reported to have a recurrence of the ventral curvature, although 10 (23%) had complications during follow-up and 9 underwent reoperations.26 With this, the present concept of STraighten And Close (STAC) hypospadias repair or the Straighten and Graft (STAG) has been popularised by Snodgrass and Bush (Figure 8).

Figure 8 The staged tubularized autograft (STAG) repair. (A) At the time of the first stage, one to three ventral corporotomies are made through the tunica albuginea, with the middle incision opposite the point of maximal curvature. (B) Preputial graft is marked and harvested. (C) Preputial graft is placed on the ventral aspect of the penile shaft and then quilted into place (D). The bottom panel displays the second stage of the repair. (E) Urethroplasty incisions are marked and extended along the midline of the scrotum. (F) Glans wings are developed. (G) Two-layer urethroplasty is performed and subsequently covered with a barrier layer with tunica vaginalis. (H) Appearance after closure [From: Snodgrass W: Staged tubularized autograft repair for primary proximal hypospadias. J Urol 198:680–686, 2017].
The flaps have the said limitation of blood supply to the edges, more chances of stricture and increased rate of diverticula formation as they are less fixed to the underlying corpora. These shortcomings are overcoming the graft technique where there is uniform supply to the graft which is well fixed to the underlying corpora and thus less chances of stricture formation and diverticula formation respectively. The flowchart by Moscardi et al is useful in individualising the management of severe penile curvature in patients with proximal hypospadias (Figure 4).22
Dorsal Plication
In some patients where the curvature still persists or there is a glans tilt only, or if the chordee is less than 30 degrees, a dorsal plication can be done, as previously popularised by Baskin. Presently, most surgeons perform the Nesbit’s or modified Nesbit’s procedure. In this technique, a diamond-shaped wedge of dorsal lateral albuginea is resected at the point of maximum curvature and the defect is sutured transversely afterwards with a non-absorbable suture like proline.27 Several modifications to this technique have been reported, including dorsal plication without resection of the penile fascia.
One-Stage Hypospadias Repair
This usually involves dorsal plication to correct ventral penile curvature in conjunction with several different urethroplasty techniques depending upon the tissue used in the repair; preputial skin; local skin; or a buccal graft.7 Some of the one staged hypospadias repair are:
Transverse preputial Island flap (Duckett tube);28 In this a preputial island flap is harvested, and tabularised it into a substitution urethroplasty. This was modified by Asopa,29 where rather than tubularising the flap before securing it to the penile shaft, the left side of the flap is anchored to the ventral surface of the penile shaft, just to the left of midline.7 Then interrupted Lembert sutures are used to close the flap in the midline. This reduces the risk of exposing the epithelium beneath the repair. The sutures are carried into the mid glans. Then, the flap is carefully placed over the suture line, and the glans wings are brought over the urethroplasty and the vascular flap. The base of the tubularized flap is anchored to the distal extent of the native urethra (Figure 9).2,7 A two-layer tubularisation is carried out, maintaining an even calibre throughout. In patients with severe curvature corrected after skin dissection and division of the urethral palpate, this approach can be helpful.7
The Onlay Island Flap procedure: OIF is indicated in boys whose curvature is corrected after penile degloving and does not require division of a relatively thin urethral plate that otherwise could not be tubularized.7 The salient features of this procedure and other one-staged hypospadias repair techniques are given below.
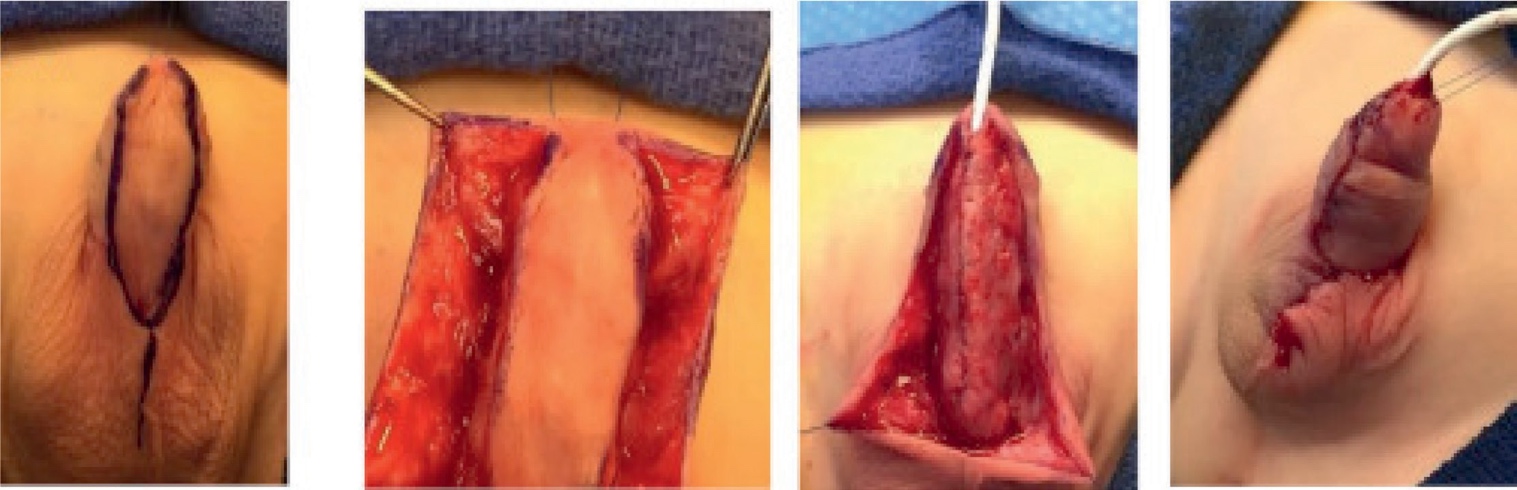
Figure 9 Island tube hypospadias repair. (A) Preoperative appearance. The pink, shiny, ventral skin suggests a thinning of the ventral spongiosum. In spite of the subcoronal meatus, this is a proximal variant. (B) After degloving the meatus is located at the penoscrotal junction and is cannulated with an 8-Fr feeding tube. (C) Artificial erection after dorsal plication reveals no residual penile curvature. (D) The preputial island flap is mobilized, with harvest of the supple dartos pedicle off of the shaft skin toward the base of the penis. (E) One edge of the flap is anchored to the tunica albuginea. (F) The flap is measured to a width of 12 mm with excision of redundant epithelium. The flap is then closed over a diversion tube, approximating the epithelial edge to the previously anchored portion of the flap. (G) Completed repair. [From Kraft KH, Shukla AR, Canning DA: Hypospadias. Urol Clin North Am 2010; 37: 167–181.]
Onlay Island Flap
- Island flap raised from inner prepuce
- The combined width of the urethral plate and flap should be 12 mm or less, and is trimmed accordingly, in particular, to narrow the proximal flap to prevent a diverticulum at the junction of the neo and native urethral anastomosis
- Blood supply of dorsal skin is not dependent on subcutaneous tissue
- Can be done in scrotal/perineal hypospadias
- No strictures
- Fistula rate decreased to 15%
Lateral Based
- In proximal hypospadias with little chordee30
- Small or flat glans
- Flap width is decided by urethral plate
- Suture the distal end of flap 2mm from tip of glans
- Left border is sutured first before separating from the right border
Tubularised Island Flap Repair
- Severe hypospadias cases when urethral plate needs to be resected
- Dorso Ventral Transfer of Tubularised plate urethroplasty (DVTPTU)
- High incidence of diverticula
- Low incidence of fistula formation
Extended Tip Urethroplasty
- Described in the setting of a boy whose curvature is corrected with skin dissection or plication in combination with an adequate urethral plate31
- Technical modifications including urethral plate mobilization and transverse corporotomies, in the setting of persistent ventral curvature of greater than 30 degrees after degloving, to increase its applicability.
- However, analysis by Snodgrass et al.32 suggested that aggressive mobilization of the urethral plate can lead to devascularization, increasing the risk of stricture formation, which ultimately limits the applicability of proximal TIP in the setting of severe hypospadias with chordee. Because of a higher risk of complications, this technique has since fallen out of favour for other two-stage repairs, such as the Byars flap or STAG repair.
Two-Staged Hypospadias Repair
Most commonly performed procedures for severe hypospadias
- Byars two staged repair:
- In stage 1
- Chordee correction
- Penile straightening with removal of the ventral tethered urethral plate is performed
- Preputial flap formed by splitting of the dorsal skin is rotated to cover ventral defect
- Open glans widely & place adequate skin flap
- In Stage 2
- The area is tabularised into a urethral tube
- Performed at least after 6 months of stage 1
- In stage 1
Shukla et al performed proximal hypospadias repair by the Byar’s flap technique in 700 boys over a period of 11 years.33 They reported fistula in 21 (3%) of these patients. None had complete disruption or urethral diverticula or meatal stenosis. In their series, age range of patients in our study was 3–12 years and the second stage was performed at least 1 year after the first surgery. The authors emphasised the advantages of a Byar’s flap: 1) being a vascularized skin flap, they found it to be a reliable when used in the first stage, and at the same time, there was abundant vascularized skin left to resurface the raw area that had been created as a result of chordee correction, 2) on completion of the procedure, a circumcised appearance was attained, 3) no contraction or loss unlike in the case of a graft were reported in their study.33
- Two-stage Bracka buccal/prepucial graft hypospadias repair34
- In stage 1 (Figure 10):
- Previous scar tissue, if any, is resected
- Glans wings mobilized
- Buccal graft or free preputial graft is quilted to cover ventral area of the resected scar
- The donor site for buccal mucosa is usually the lip or the cheek
- Suturing of the mucosal defect after the removal of the graft is not recommended.
- In Stage 2:
- The plate is tabularised, usually done after 6 months
- Good procedure for re-doing urethroplasties
- In stage 1 (Figure 10):
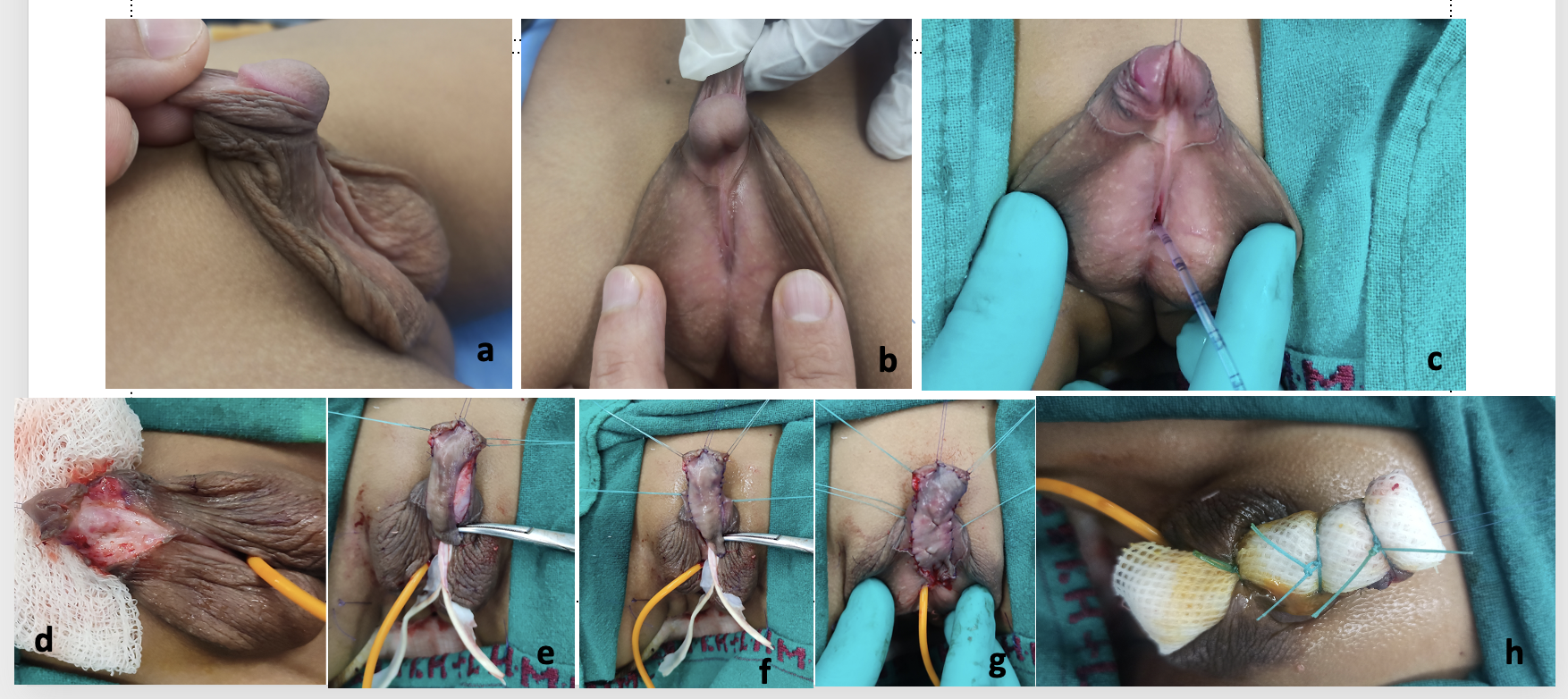
Figure 10 Courtesy Dr. Vikram Khanna, Associate Professor , Pediatric Surgery, Lady Harding Medical College and Kalawati Saran Children’s Hospital, New Delhi, a) Pre-operative pic showing penoscrotal hypospadias with penoscrotal transposition, chordee and short phallus with dorsal hooded prepuce, b) Lateral profile showing the degree of chordee and the urethral plate, c) feeding tube inserted as stent using double catheter method
d) Degloving of the penile shaft and correction of chordee, e) Prepucial skin graft harvested, f) Graft sutured to the area of the split glans wings and the area of urethral plate and corporal body, g) Complete fixation of graft with quilting performed, h) Tie over dressing done over the graft and catheter left in situ for 1 week.
Bracka described the concept of 2 stage hypospadias repair.34 After at least 6 months of the first stage of repair, the second stage can be performed. During this repair, any remaining chordee is corrected, tubularisation of the graft is performed, neourethra created, meatoplasty, and glansplasty done. The urethroplasty is covered by a dartos flap or a tunica vaginalis flap. In today’s era, it has become widely accepted as a primary treatment for patients with proximal hypospadias and chordee. In Bracka’s series of pediatric two staged hypospadias repair which included 457 children (369 primary repair and 88 secondary or salvage repairs) and 143 adults (22 primary and 121 secondary), 5.7%35 developed urethrocutaneous fistulae, 7%14 developed strictures, and 4.6%29 developed late onset of strictures.34,35
The use of the skin from the inner prepuce is an excellent option as the graft is thin, flexible, hairless, and withstands a moist environment. The graft is harvested and the dartos layer is removed and anastomosed ventrally to the corpora to form the neourethral plate. Tubularization of the graft is generally performed later, after 6 months. One of the problems
with foreskin graft is the availability of this graft. This is because many patients with proximal hypospadias and ventral curvature have scarce penile skin and, all the skin is needed and used for resurfacing of the penis in the initial stage. Although the use of grafts for hypospadias repair was mostly used for reoperations, some series have reported good outcomes with staged repair using preputial grafts for primary proximal hypospadias correction also.36,37
In cases where preputial skin cannot be used or is unavailable, the buccal mucosa (Figure 11) is harvested from the inner cheek and/or lower labial alveolar region and grafted to the corpora. Its properties include increased elastin, relative stiffness providing good support and ultimately diminishing the occurrence of urethral diverticulum and meatal prolapse,38,39 making it suitable for its use in hypospadias surgery. During harvesting of buccal mucosal graft, one should avoid crossing the angle of the mouth into the lower lip, thus avoiding cosmetic facial deformities. Secondly, care should be taken to avoid the Stensen’s duct when harvesting the mucosa from the inner cheek.
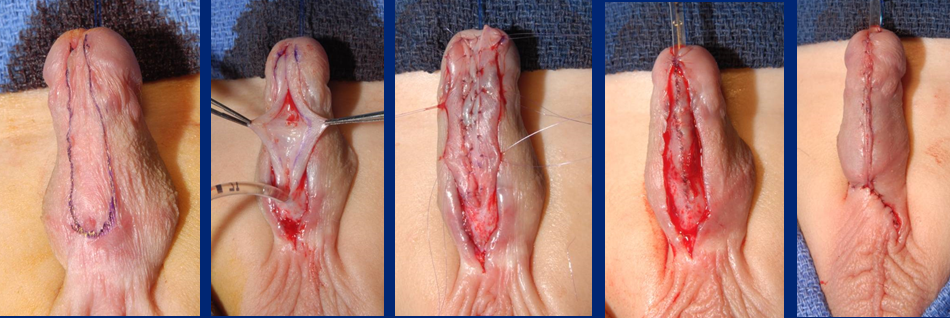
Figure 11 Tubularization of graft inlay of Buccal Mucosal Graft
Based on the available literature, preputial graft in primary cases is the preferred method, the other available grafts are the lingual graft and buccal mucosal grafts.40,41 In proximal hypospadias cases, most of the time, we can use the preputial mucosa, which is not really preputial skin, that is shiny , as a graft, and we don’t find skin deficiency in the first stage, since we are not covering the penis with skin in the first stage of graft placement.
In a series of 43 boys who completed both stages with postoperative follow up, Snodgrass and Bush concluded that staged tubularised autograft resulted in a straight penis with a normally positioned neo meatus in boys with the most severe proximal hypospadias in 77%.26 This number increased to 98% after 1 or 2 reoperations for complications. In their series, they also found no recurrence of ventral curvature after 3 corporotomies without corporal grafting had been performed [Snodgrass]. The mean ventral curvature for these penises was 70 degrees, and corporotomy was performed in 65%, the preputial grafts were used in 88%.26
Postoperative Management and Care
Urinary Drainage
Drainage should be ensured by an infant feeding tube left in situ post-repair. We generally use a 6F or 8F IFT for young children and a 10F to 12F for older children, adolescents and adults. Care should be taken to place the tip of the stent inside the bladder such that there are no bladder spams due to the irritation of the trigone and there is no internal knotting due to excessive length of the catheter left inside. The best thing is to use a silicone catheter.
Dressing
The dressing is applied in a circular fashion around the penile shaft after adequate padding over the repaired scrotal region. It should neither be too tight, nor too loose and the glans tip should be visible or exposed for visual inspection during the post-operative period.
Another alternative could be to apply dressing and secure it to the abdominal wall with sterile plastic dressing or a sandwich dressing with Elastoplast.
During staged repair, when using the graft in the first stage, we use a tie over dressing (Figure 10), to fix the graft, and this is removed one week later. The graft below is fixed to the underlying corporal body by quilting sutures. The tie over dressing helps obliterate any free space between the graft and the underlying corpora, sweep out the excess fluid and aids in better apposition of the graft tissue.
Complications
The brief overview of the main complications post repair can be either related to urethroplasty or skin complications.7
Urethroplasty Complications
- Fistula
- Glans dehiscence
- Meatal stenosis obstructive symptoms (straining, prolonged voiding, urinary tract infection, and/or retention)
- Urethral stricture
- Urethral diverticulum
Skin Complications
- Skin necrosis
- Penile torsion > 30 degrees- angle between the normal and true vertical glanular plane >30 degrees from midline (specify clockwise or counterclockwise)
- Preputial fistula - fistula-like defect in the preputial skin that has no contact with the urethral lumen
- Preputial dehiscence after preputial reconstruction: defect in the preputial skin recreating an incomplete prepuce
- Lichen sclerosus
These could also be defined as early in the form of glans ischaemia, preputial flap necrosis, catheter blockage, premature expulsion of catheter and wound infection. The late complications include urethrocutaneous fistula formation, glans dehiscence, meatal stenosis, recurrent or residual chordee, urethral stricture, urethral dehiscence and urethral diverticulum.
Table 3 The complications of various 2-stage graft studies have been highlighted, a 48 (out of 140) patients only were managed with two-stages using preputial graft, b 15 (30%) patients had multiple complication, c 44 were primary cases with 8 being redo.
| Study | Number patients | Mean follow up (months) | Meatal location | Repair type | Overall complications (%) | Meatal stenosis (%) | Dehiscence (%) | Stricture (%) | Urethral diverticulae (%) | Fistula (%) | Residual curvature (%) | Other |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ferro, 200236 | 34 | 1–48 (range) | proximal | 2-stage preputial graft | 8 (24%) | 0 | 4 (11.7%) | 1 (3%) | 1 (3%) | 2 (6%) | — | — |
| Johal, 200637 | 62 | 26 (median) | midshaft / proximal | 2-stage graft | 11 (18%) | 3 (5%) | 3 (5%) | 0 | 0 | 0 | 3 (5%) | Deviated stream 2 (3%) |
| Pippe Salle, 201614 | 48a | 29.6 (median) | proximal | 2-stage graft | 16 (33.3%) | 0 | 7 (14.5%) | 1 (2%) | 1 (2%) | 5 (10.4%) | 2 (4.1%) | — |
| Faure, 201642 | 52 | 34 (median) | proximal / redoc | 2-stage graft (preputial/BMG) | 20 (38.4%) | 8 (15.3%) | 1 (1.9%) | 4 (7.6%) | 1 (1.9%) | 8 (15.3%) | 0 | — |
| Sakr, 201743 | 23 | 12 | redo | 2-stage (lingual graft) | 3 (13%) | 0 | 1 | 0 | 0 | 2 | 0 | — |
| Snodgrass, 201726 | 43 | 22 | proximal | 2-stage | 10 (24%) | 0 | 7 (16.2%) | 0 | 1 (2.3%) | 2 (4.6%) | 0 | — |
| Lanciotti, 201740 | 50 | 63.6 | proximal | 2-stage (bladder graft) | 23 (46%)b | 4 (8%) | 0 | 15 (30%) | 6 (12%) | 9 (18%) | 5 (10%) | Prolapse of meatus 7 (14%) |
Table 4 The complications of various 2-stage flap repair studies have been highlighted. a combined 2-stage technique with distal TIP and tubularized Byars flap, b - VC reassessed during the 2-stage with an artificial erection, c 37 were staged in 2 procedures, d 6 had bladder tube, buccal grafts etc, e 12 (out of 140) patients only were managed with two-stages preputial flaps, f 81 (out of 167) patients were managed with two-stages preputial flaps, TPIF=transverse preputial island flap; BILAB=bilateral based skin flap.
| Study | Number patients | Mean follow-up (months) | Meatal location | Repair type | Overall complications (%) | Meatal stenosis (%) | Dehiscence (%) | Stricture (%) | Urethral diverticulae (%) | Fistula (%) | Residual curvature (%) | Other |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Greenfield, 199444 | 39 | 16 | Subglanular to perineal | 2-stage flap (belt-fuqua) | 16 (41%) | 0 | 0 | 7 (17.9%) | 8 (20.5%) | 1 (2.5%) | — | - |
| Retik, 199445 | 58 | — | Scrotal/perineal | 2-stage flap | 3 (5%) | 0 | 0 | — | — | 3 (5%) | — | - |
| Cheng, 200346 | 14 | 6–36 (range) | proximal | 2-stagea | 4 (28.5%) | 0 | 0 | 0 | 2 (14%) | 1 (7%) | 0b | Meatal recession 1 (7%) |
| Hadidi, 201439 | 63c | 43 | perineal | 1-stage/2-stage BILAB | 9 (14.2%) | — | 3 (4.7%) | — | 2 (3%) | 1 (1.5%) | — | Scar contraction 3 (4.7%) |
| McNamara, 201547 | 134d | 45.6 (median) | proximal | 2-stage flap | 71 (53%) | 17 (12.7%) | 19 (14.2%) | 16 (11.9%) | 12 (9%) | 39 (29.1%) | 3 (2.2%) | - |
| Stanasel, 201548 | 56 | 38.6 | proximal | 2-stage flap | 38 (68%) | 5 (9%) | 3 (5%) | 8 (14%) | 8 (14%) | 32 (57%) | — | - |
| Tiryaki, 201649 | 34 | 44.8 | proximal | 2-stage Byars flap | 32 (95%) | 0 | 0 | 0 | 24 (70%) | 23 (67%) | 1 (3%) | 27 urethral prolapse |
| Pippe Salle, 201614 | 12e | 29.6 | proximal | 2-Stage flap | 4 (41.6%) | 0 | 3 (25%) | — | 0 | 2 (16.6%) | 1 (8.3%) | - |
| Chen, 201650 | 87 | TPIF - 38 (median)Byars – 36 (median) | proximal | Staged TPIF,42 2-Stage Byars flap45 | TPIF 9.5%, Byars 33% | — | 0, 3 (6.6%) | 1 (2.3%), 2 (4.4%) | 1 (2.3%), 0 | 2 (4.6%), 10 (22.2%) | 0b,0b | - |
| Long, 201736 | 81f | 27.7 (median) | proximal | 2-Stage Byars flap | 40 (49%) | 5 (6%) | 6 (7%) | — | 5 (6%) | 30 (37%) | 3 (4%) | - |
| Jayanthi, 201737 | 34 | 15.2 | proximal | Modified Ulaanbaatar | 5 (14.7%) | 0 | 0 | 0 | 4 (12%) | 0 | — | Recurrent epididymitis 1 (2.7%) |
In a study conducted at The Children’s Hospital of Philadelphia (CHOP) from 1996–2006, which compared the results for 665 consecutive boys who underwent hypospadias repair, found that the complication rate for all hypospadias was 17%.51 Of the 665, 86 (13%) had proximal hypospadias, defined by the location of the urethral meatus proximal to the midshaft after penile degloving in the operating room. They observed a disproportionate number of complications (35%) occurred in the boys with proximal hypospadias, with a proximal hypospadias complication rate of 39/86 (45%).51 This contrasted sharply with the 17% overall complication rate.51
Most proximal hypospadias repair patients require a longer and closer follow-up for a detailed and honest reporting of complications. A hypospadias criple can be defined as a boy who often requires multiple, complex procedures to correct the sequelae of a failed initial repair.52 Due to the longer urethroplasty tube, there is a greater the risk for stricture or a profound effect of the failure of the reconstructed urethra to expand with voiding, increasing resistance to urine flow, ultimately resulting in fistula and/or urethral diverticulum formation as highlighted by Braga et al.53 Hence there has been underreporting of the complications for proximal hypospadias previously.
To improve the outcomes of repair of proximal hypospadias, Long and Canning51 pointed that a standardized system to systematically quantify the severity of the hypospadias phenotype so as to create a universal hypospadias language that would facilitate collaboration across institutions can be used. Presently, the scoring systems used are the HOSE, HOPE, and GMS13,54 which include various factors like the glans width, degree of penile curvature, and quality of urethral plate to for a given patient and calculate a particular score. This has to an extent simplified comparison for outcome analysis, barring a few patient related and inter-observer surgeon limitations.
They also highlighted the importance of the patient and family assessment being collated with surgeon analysis after surgical intervention51 as they may not always match. The penile perception score takes into account this limitation.55 Weber et al55 in their study evaluated 77 boys (6–17 years old) who had undergone hypospadias repair regarding their penile self-perception with regard to the meatus, glans, skin and general appearance. They found that the inter-correlation of these items “meatus,” “glans” and “skin” with “general appearance” was good among the boys, parents and urologists. Patients with hypospadias expressed high satisfaction with the penile appearance, which did not differ significantly from their age-matched controls. Interestingly, however, the parents and urologists were less satisfied with the penile appearance than were the patients themselves.55 This highlights the importance of self-assessment by the patient and the parents, apart from the operating surgeon.
Another method suggested by Long et al is by coaching and teamwork51 utilizing various opportunities like meetings, conference, workshops, critical analysis of recorded videos in a closed group, feedback and discussion. This would definitely increase exposure and advance understanding of this complex and rare disease of proximal hypospadias.
References
- Baskin LS. Chapter 121 - Hypospadias. In: Coran AG, In, editors. Pediatric Surgery (Seventh Edition). Mosby; 2012. DOI: 10.1016/b978-0-323-07255-7.00121-5.
- Samuel M, Capps S, Worth A. Proximal Hypospadias. Eur Urol 2011; 40 (4): 463–468. DOI: 10.1159/000049817.
- Baskin L, Erol A, Jegatheesan P, Li Y, Liu W, Cunha G. Urethral seam formation and hypospadias. Cell Tissue Res 2001; 305 (3): 379–387. DOI: 10.1007/s004410000345.
- Baskin L, Shen J, Sinclair A, Cao M, Liu X, Liu G, et al.. Development of the human penis and clitoris. Differentiation 2018; 103: 74–85. DOI: 10.1016/j.diff.2018.08.001.
- Smith DR, Tanagho EA, McAninch JW. Smith’s General Urology. Norwalk, Conn: Appleton & Lange; Chap; 1992.
- Wein AJ, Kavoussi LR, Campbell MF. 1. 2012.
- Gerasaro TS, Brock WA, Kaplan GW. Upper Urinary Tract Anomalies Associated With Congenital Hypospadias: Is Screening Necessary? J Urol 1986; 135 (3): 537–538. DOI: 10.1016/s0022-5347(17)45729-6.
- Rajfer J, Walsh PC. The Incidence of Intersexuality in Patients with Hypospadias and Cryptorchidism. J Urol 1976; 116 (6): 769–770. DOI: 10.1016/s0022-5347(17)59004-7.
- Kaefer M, Diamond D, Hendren WH, Vemulapalli S, Bauer SB, Peters CA, et al.. The Incidence Of Intersexuality In Children With Cryptorchidism And Hypospadias: Stratification Based On Gonadal Palpability And Meatal Position. J Urol 1999; 162 (3 Part 2): 1006–1007. DOI: 10.1016/s0022-5347(01)68049-2.
- Ahmed SF, Achermann JC, Arlt W, Balen A, Conway G, Edwards Z. Society for Endocrinology UK guidance on the initial evaluation of an infant or an adolescent with a suspected disorder of sex development. 2015; 4 (5): 71–88. DOI: 10.1111/j.1365-2265.2011.04076.x.
- Hadidi AT, Azmy AF. Hypospadias surgery: an illustrated guide. 2004. DOI: 10.1111/j.1440-1754.2005.571_3.x.
- Shoor G, Acharya SK. Bedside clinics and Round questions in Pediatric Surgery. 2022.
- Arlen AM, Kirsch AJ, Leong T, Broecker BH, Smith EA, J.M.. Faculty Opinions recommendation of Further analysis of the Glans-Urethral Meatus-Shaft (GMS) hypospadias score: correlation with postoperative complications. Faculty Opinions – Post-Publication Peer Review of the Biomedical Literature 2015; 11. DOI: 10.3410/f.725403208.793522967.
- Abbott JE, Heinemann A, Badalament R, Davalos JG. A clever technique for placement of a urinary catheter over a wire. Urol Ann 2015; 7 (3): 367. DOI: 10.4103/0974-7796.157959.
- Hughes IA, Houk C, Ahmed SF, Lee PA, Group LWPESC, Group ESPEC. Consensus Statement on Management of Intersex Disorders. Pediatric Clinical Practice Guidelines &Amp; Policies 2006; 91 (7): 1317–1317. DOI: 10.1542/9781610021494-part06-consensus_statement2.
- Urology S on. Timing of Elective Surgery on the Genitalia of Male Children With Particular Reference to the Risks, Benefits, and Psychological Effects of Surgery and Anesthesia. Pediatrics 1996; 97 (4): 590–594. DOI: 10.1542/peds.97.4.590.
- Bermudez DM, Canning DA, Liechty KW. Age and pro-inflammatory cytokine production: Wound-healing implications for scar-formation and the timing of genital surgery in boys. J Pediatr Urol 2011; 7 (3): 324–331. DOI: 10.1016/j.jpurol.2011.02.013.
- Belman AB, Kass EJ. Hypospadias Repair in Children Less than 1 Year Old. J Urol 1982; 128 (6): 1273–1274. DOI: 10.1016/s0022-5347(17)53458-8.
- Hadidi AT. History of hypospadias: Lost in translation. J Pediatr Surg 2017; 52 (2): 211–217. DOI: 10.1016/j.jpedsurg.2016.11.004.
- Snodgrass W, Prieto J. Straightening Ventral Curvature While Preserving the Urethral Plate in Proximal Hypospadias Repair. J Urol 2009; 182 (4s): 1720–1725. DOI: 10.1016/j.juro.2009.02.084.
- Moscardi PRM, Gosalbez R, Castellan MA. Management of High-Grade Penile Curvature Associated With Hypospadias in Children. Front Pediatr 2017; 5 (189). DOI: 10.3389/fped.2017.00189.
- Braga LHP, Pippi Salle JL, Dave S, Bagli DJ, Lorenzo AJ, Khoury AE. Outcome Analysis of Severe Chordee Correction Using Tunica Vaginalis as a Flap in Boys With Proximal Hypospadias. J Urol 2007; 178 (4s): 1693–1697. DOI: 10.1016/j.juro.2007.03.166.
- Gittes RF, McLaughlin AP. Injection technique to induce penile erection. Urology 1974; 4 (4): 473–474. DOI: 10.1016/0090-4295(74)90025-9.
- Castellan M, Gosalbez R, Devendra J, Bar-Yosef Y, Labbie A. Ventral corporal body grafting for correcting severe penile curvature associated with single or two-stage hypospadias repair. J Pediatr Urol. 2011;7:289-93. . DOI: 10.1016/j.jpurol.2012.02.009.
- Snodgrass W, Bush N. Staged Tubularized Autograft Repair for Primary Proximal Hypospadias with 30-Degree or Greater Ventral Curvature. J Urol 2017; 198 (3): 680–686. DOI: 10.1016/j.juro.2017.04.019.
- Nesbit RM. Operation for Correction of Distal Penile Ventral Curvature with or Without Hypospadias. J Urol 1966; 97 (4): 720–722. DOI: 10.1016/s0022-5347(17)63105-7.
- Duckett JW. Transverse Preputial Island Flap Technique for Repair of Severe Hypospadias. Urol Clin North Am 1980; 7 (2): 423–430. DOI: 10.1016/s0094-0143(21)01243-x.
- Ascopa HS, Elhence IP, Atri SP, Bansal NK. One stage correction of penile hypospadias using a foreskin tube. Plast Reconstr Surg 1971; 49 (1): 104–105. DOI: 10.1097/00006534-197201000-00044.
- Hypospadias Surgery: Science and Art - V.V.S. . DOI: 10.4103/jiaps.jiaps_202_20.
- Snodgrass WT, Lorenzo A. Tubularized incised-plate urethroplasty for proximal hypospadias. BJU Int 2002; 89 (1): 90–93. DOI: 10.1046/j.1464-410x.2002.02524.x.
- Snodgrass WT, Granberg C, Bush NC. Faculty Opinions recommendation of Urethral strictures following urethral plate and proximal urethral elevation during proximal TIP hypospadias repair. Faculty Opinions – Post-Publication Peer Review of the Biomedical Literature 2013; 9 (6 Pt B): 990–994. DOI: 10.3410/f.718013467.793494058.
- Singh AP, Shukla AK, Sharma P, Shukla J. Two stages repair of proximal hypospadias: Review of 700 cases. J Indian Assoc Pediatr Surg 2017; 22 (3): 158. DOI: 10.4103/0971-9261.207627.
- Bracka A. Hypospadias repair: the two-stage alternative. Br J Urol 1995; 76 (6): 31–41. DOI: 10.1111/j.1464-410x.1995.tb07815.x.
- Bracka A. Buccal Mucosa: Good But Not Perfect. J Urol 2011; 185 (3): 777–778. DOI: 10.1016/j.juro.2010.12.015.
- FERRO F, ZACCARA A, SPAGNOLI A, LUCCHETTI MC, CAPITANUCCI ML, VILLA M. Skin Graft for 2-stage Treatment of Severe Hypospadias: Back to the Future? J Urol 2002; 168 (4 Pt 2): 1730–1733. DOI: 10.1097/00005392-200210020-00018.
- Johal NS, Nitkunan T, O’Malley K, Cuckow PM. The Two-Stage Repair for Severe Primary Hypospadias. Eur Urol 2006; 50 (2): 366–371. DOI: 10.1016/j.eururo.2006.01.002.
- Dessanti A, Rigamonti W, Merulla V, Falchetti D, Caccia G. Autologous Buccal Mucosa Graft for Hypospadias Repair: An Initial Report. J Urol 1992; 147 (4): 1081–1083. DOI: 10.1016/s0022-5347(17)37478-5.
- Hadidi AT. Perineal Hypospadias: The Bilateral-Based (BILAB) Skin Flap Technique. Hypospadias Surgery 2014; 49 (1): 497–506. DOI: 10.1007/978-3-030-94248-9_32.
- Lanciotti M, Betti M, Elia A, Landi L, Taverna M, Cini C, et al.. Proximal hypospadias repair with bladder mucosal graft: Our 10 years experience. J Pediatr Urol 2017; 13 (3): 294.e1–294.e6. DOI: 10.1016/j.jpurol.2017.01.011.
- Pal DK, Gupta DK, Ghosh B, Bera MK. A comparative study of lingual mucosal graft urethroplasty with buccal mucosal graft urethroplasty in urethral stricture disease: An institutional experience. Urol Ann 2016; 8 (2): 157. DOI: 10.4103/0974-7796.172214.
- Pippi Salle JL, Sayed S, Salle A, Bagli D, Farhat W, Koyle M, et al.. Proximal hypospadias: A persistent challenge. Single institution outcome analysis of three surgical techniques over a 10-year period. J Pediatr Urol 2016; 12 (1): 28.e1–28.e7. DOI: 10.1016/j.jpurol.2015.06.011.
- Faure A, Heloury Y. Response to “Re: Faure A, Bouty A, Nyo L, O’Brian M, Heloury Y. Two-stage graft urethroplasty for proximal and complicated hypospadias in children: a retrospective study.” J Pediatr Urol 2016; 12 (5): 286 1–286 7. DOI: 10.1016/j.jpurol.2016.12.007.
- Sakr A, Elkady E, Abdalla M, Fawzi A, Kamel M, Desoky E, et al.. Lingual mucosal graft two-stage Bracka technique for redo hypospadias repair. Arab J Urol 2017; 15 (3): 236–241. DOI: 10.1016/j.aju.2017.06.002.
- Greenfield SP, Sadler BT, Wan J. The Two-Stage Repair for Severe Primary Hypospadias. Yearbook of Urology 1994; 2007 (2 Pt 1): 250. DOI: 10.1016/s0084-4071(08)70198-2.
- Retik AB, Bauer SB, Mandell J, Peters CA, Colodny A, Atala A. Management of Severe Hypospadias with a 2-Stage Repair. J Urol 1994; 152 (2 Part 2): 749–751. DOI: 10.1016/s0022-5347(17)32697-6.
- CHENG EARLY, KROPP BRADLEYP, POPE JOHNC, BROCK JOHNW. Proximal Division of the Urethral Plate in Staged Hypospadias Repair. J Urol 2003; 170 (4 Part 2): 1580–1584. DOI: 10.1097/01.ju.0000084258.93064.f4.
- Canning D. Faculty Opinions recommendation of Management of Proximal Hypospadias with 2-Stage Repair: 20-Year Experience. Faculty Opinions – Post-Publication Peer Review of the Biomedical Literature 2015; 194 (4): 1080–1085. DOI: 10.3410/f.725486894.793522961.
- Canning D. Faculty Opinions recommendation of Complications following Staged Hypospadias Repair Using Transposed Preputial Skin Flaps. Faculty Opinions – Post-Publication Peer Review of the Biomedical Literature 2015; 194 (2): 512–516. DOI: 10.3410/f.725364224.793522958.
- Tiryaki S, Əl\Elzschwakb\Elzschwarova VE, Dokumcu Z, Ergun R, Tekin A, Yagmur I, et al.. Unexpected outcome of a modification of Bracka repair for proximal hypospadias: High incidence of diverticula with flaps. J Pediatr Urol 2016; 12 (6): 395.e1–395.e6. DOI: 10.1016/j.jpurol.2016.04.046.
- Lin H, Wang Y-Y, Li S-B, Chen Z-T, Su L-J. Staged transverse preputial island flap urethroplasty for some proximal hypospadias with moderate-to-severe chordee. BMC Urol 2016; 21 (1): 1536–1540. DOI: 10.1186/s12894-021-00948-8.
- Hanna M. Faculty Opinions recommendation of Hypospadias: Are we as good as we think when we correct proximal hypospadias? Faculty Opinions – Post-Publication Peer Review of the Biomedical Literature 2016: 1477513116300432–. DOI: 10.3410/f.726422269.793519822.
- Barbagli G, Sansalone S, Djinovic R, Lazzeri M. Surgical Repair of Late Complications in Patients Having Undergone Primary Hypospadias Repair during Childhood: A New Perspective. Adv Urol 2012; 2012 (705212): 1–5. DOI: 10.1155/2012/705212.
- Braga LH, Pippi Salle JL, Lorenzo AJ. Comparative Analysis of Tubularized Incised Plate Versus Onlay Island Flap Urethroplasty for Penoscrotal Hypospadias. Yearbook of Urology 2007; 2008 (1451-6): 246–247. DOI: 10.1016/s0084-4071(08)79119-x.
- Holland AJA, Smith GHH, Ross FI, Cass DT. HOSE: an objective scoring system for evaluating the results of hypospadias surgery. BJU Int 2001; 88 (3): 255–258. DOI: 10.1046/j.1464-410x.2001.02280.x.
- Merriman LS, Arlen AM, Broecker BH, Smith EA, Kirsch AJ, Elmore JM. The GMS hypospadias score: Assessment of inter-observer reliability and correlation with post-operative complications. J Pediatr Urol 2013; 9 (6): 707–712. DOI: 10.1016/j.jpurol.2013.04.006.
- F T, TP J, RP G. RE: Introducing the HOPE (Hypospadias Objective Penile Evaluation)-score: A validation study of an objective scoring system for evaluating cosmetic appearance in hypospadias patients. J Pediatr Urol 2013; 9 (6): 1016. DOI: 10.1016/j.jpurol.2013.07.022.
- Weber DM, Schonbucher VB, Landolt MA, Gobet R. Faculty Opinions recommendation of The Pediatric Penile Perception Score: an instrument for patient self-assessment and surgeon evaluation after hypospadias repair. Faculty Opinions – Post-Publication Peer Review of the Biomedical Literature 2008; 180 (1080-4): 1084. DOI: 10.3410/f.719560881.793500484.
最近更新时间: 2024-02-16 20:59