39: Urogenital Sinus
Este capítulo levará aproximadamente 12 minutos para ler.
Introduction
Isolated urogenital sinus is a rare congenital abnormality of the female urogenital system where the urethra and vagina fail to separate during development, forming a common channel. Urogenital sinus anomalies are found in four different clinical scenarios:1
- Genital ambiguity states (such as congenital adrenal hyperplasia)
- Persistent cloaca with rectal involvement
- Female exstrophy
- Isolated urogenital sinus
This chapter will focus on isolated urogenital sinus.
Epidemiology
The incidence of isolated urogenital sinus is not well known, although sources report an incidence rate ranging from 6/100,000 to 1/250,000 female births.2,3
Embryology/Etiology
The common urogenital sinus (UGS) is a normal transient structure in embryonic development that later separates and gives rise to the urethra and distal third of the vagina. The etiology of isolated urogenital sinus is not well understood but generally accepted to be the result of an arrested development of female urogenital formation in the first trimester where the urethra and vagina fail to form separate perineal openings.4 It is postulated that an early arrest of vaginal differentiation will form a long common channel (high confluence), whereas a later arrest of differentiation will form a short common channel (low confluence) (Figure 1).5
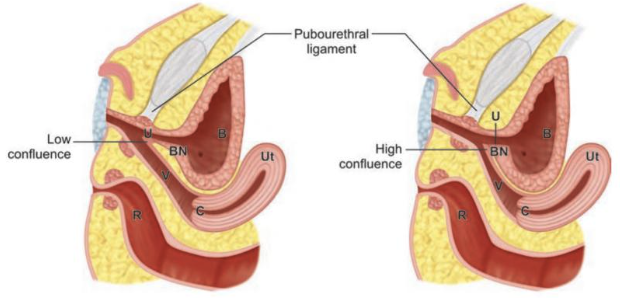
Figure 1 Diagram depicting low confluence (left) and high confluence (right). Note the location of the confluence of urethra (U) and vagina (V) in relation to the bladder neck (BN) and pubourethral ligament. Other structures depicted include the uterus (Ut), bladder (B), rectum (R), and cervix (C). Carrasco “Surgical Techniques in Pediatric and Adolescent Urology”.6
Clinical Evaluation
Clinical Presentation
Many cases are identified through antenatal ultrasonography showing fluid-filled pelvic structures that often represent hydrocolpos or hydrometrocolpos (Figure 2).1,6
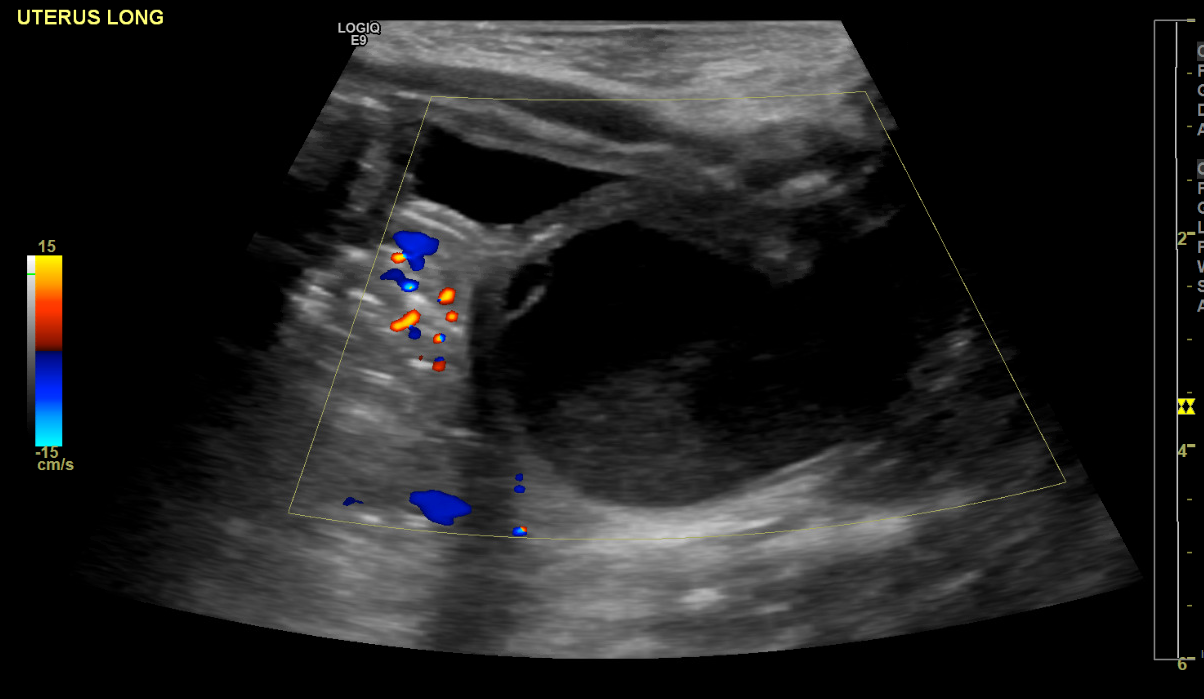
Figure 2 Ultrasound showing the bladder anteriorly and hydrocolpos posteriorly.
Presenting signs and symptoms: patients that are not identified on antenatal ultrasound may later present with the following:
- Urinary tract infection
- Urinary incontinence
- Post-void dribbling
- Vaginal fluid accumulation
- Menstrual hematuria7
- Or may be asymptomatic
Physical Examination
Physical examination should include:
- Abdominal exam
- May reveal a palpable suprapubic mass representing a distended bladder and/or hydrometrocolpos1
- Spinal exam
- Lower spine exam should be completed as urogenital sinus anomalies can be associated with spinal cord abnormalities1
- Genital exam
- Will show a single perineal opening (Figure 3)
- For examining infants, the use of cotton tipped applicators can assist in separating the labia to appropriately visualize the perineal opening.
Figure 3 Single perineal opening on genital exam. Image adapted from Grey’s Anatomy, plate 1119 (image in public domain).
Diagnostic Testing
Imaging
The role of imaging in the workup of isolated urogenital sinus is limited. Ultrasound imaging of the urinary system and reproductive system should be completed to rule out any other abnormalities and to define the location of those organs.1
A genitogram can be obtained to further delineate anatomy but may be of limited utility in isolated urogenital sinus.
Spinal imaging may be needed to evaluate for spinal cord anomalies.
Endoscopy
The most critical diagnostic tool in isolated urogenital sinus is cystoscopy and vaginoscopy. This allows the surgeon to evaluate the length of the common channel and the location of the urethral and vaginal confluence in relation to the bladder neck, which is crucial in determining the appropriate surgical approach.6 This endoscopic evaluation is done at the time of surgical repair and will be discussed further in a later section of this chapter.
Surgical Management
Immediate Management
If a patient requires drainage of hydrocolpos, a catheter per common channel (intermittently or indwelling), suprapubic catheter or vaginostomy can be placed under anesthesia. Otherwise, urine will likely continue to accumulate in the vagina and/or uterus. Catheterization may be necessary until later reconstructive repair.
Definitive Management
Surgical Indications
Surgical repair is indicated if patients are symptomatic from the urogenital sinus, especially if there are issues with urine accumulation such as hydronephrosis or hydrocolpos.6 If patients are asymptomatic, surgical repair may be deferred.
Preoperative Counseling
Surgical Goals
The goals of surgical repair should be discussed with the parents before proceeding and should include the following:
- normal-appearing genitalia
- separate urethral and vaginal openings
- drainage of urine
- adequate size vaginal opening for menstrual products and future intercourse
Surgical Timing
We recommend surgical repair to be done between 6 months and 12 months of age.6 The optimal timing for isolated urogenital sinus has not been established in the literature and is extrapolated from patients with congenital adrenal hyperplasia and associated urogenital sinus.
Those that favor early surgical repair posit that the tissues may be more pliable at an early age and residual circulating maternal estrogen may promote wound healing.1 Those that favor surgical repair at age of puberty promote the same hormonal benefits in addition to the patient’s participation and assent in proceeding.1
Surgical Techniques
Preoperative Preparation
- Bowel preparation is not necessary
- Preoperative antibiotics should be given to cover skin and vaginal flora
- Surgical repair involves 2 distinct portions:
- Endoscopic evaluation to determine the length of the channel and its relation to the bladder neck
- Definitive repair via vaginoplasty
- The approach to vaginoplasty is determined by the endoscopic evaluation
Exam Under Anesthesia and Cystoscopy and Vaginoscopy
The patient should be positioned in a dorsal lithotomy position. The examination under anesthesia (EUA) should include evaluating the introitus and single perineal opening.
Next, endoscopic evaluation should be completed. During this, the surgeon should measure the length of certain anatomic parameters, such as the length of the urethra, vagina, and common channel in relation to the bladder neck. The length of the channel and its relation to the bladder neck are the most crucial parameters in determining the surgical approach to definitive repair.
- Channel length of < 3 cm → Flap vaginoplasty or PUM/TUM
- Channel length of > 3 cm → Pull-Through vaginoplasty or Anterior Sagittal Transrectal Approach (ASTRA)
Endoscopic evaluation should start with cystoscopy with the appropriately-sized rigid cystoscope. The cystoscope should be advanced through the common channel, into the urethra, which will be the anterior opening, and then into the bladder. The bladder should be thoroughly inspected to ensure there are no other anatomic abnormalities.
Then vaginoscopy is performed with the cystoscope. The general size, elasticity, and shape (ie duplication anomalies) should be evaluated.6
Once the EUA and endoscopic evaluation are complete, the surgeon should then determine which vaginoplasty approach is most appropriate for the patient.
Total and Partial Urogenital Mobilization
First described by: Alberto Pena in 19979
Indications: Adequate urethral length, extensive dissection at the level of the bladder neck not anticipated
Position: variable, depending on the method of vaginoplasty
Brief description: The entire sinus is dissected circumferentially and mobilized toward the perineum.1
This is categorized as partial urogenital mobilization (PUM) or total urogenital mobilization (TUM) depending on transection of the pubourethral ligament (Figure 4).6 This procedure also allows for mobilization of the entire sinus to provide a mucosa-lined vestibule. It enables a mid-level confluence to reach the perineum without requiring vaginal separation.
Steps
- The UGS is marked circumferentially at its junction with the labia minora and down the midline of the perineum toward the anterior border of the anus
- The dissection begins on the posterior wall of the UGS, extending laterally and then anteriorly until the UGS is circumferentially mobilized
- The lateral and anterior wall dissection should stay medial to the bulbospongiosus muscle to avoid bleeding
- Mobilization should be continued until the urethra and vagina can reach the introitus with minimal to no tension6
- Partial urogenital mobilization stops at the level of the pubourethral ligament to reduce possible risk of stress incontinence or foreshortening of the vagina (Figure 4)
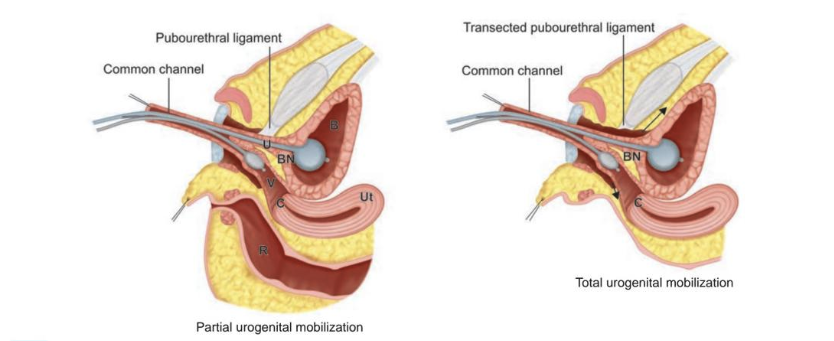
Figure 4 Partial (left) and total (right) urogenital mobilization with catheters in the bladder (B) and vagina (V) to aid with traction. Note that in total urogenital mobilization, the pubourethral ligament is transected and dissection is carried proximal (arrows) until the urethra and vagina can reach the perineum. Other structures depicted include the uterus (Ut), bladder neck (BN), and rectum (R). Source: Carrasco “Surgical Techniques in Pediatric and Adolescent Urology”.6
Flap Vaginoplasty
First described by: Fortunoff et al in 196410
Indications: low confluence, short common channel
Position: lithotomy
Brief description: The introitus and urogenital sinus are widely opened; the level of confluence does not change
During this procedure, the posterior walls of the sinus and vagina are opened, the anterior wall of the vagina is left intact, and the posterior perineal flap fits into the opened vagina; therefore, skin is covering the posterior aspect of the introitus and vaginal wall.
Steps
- An inverted U or omega-shaped incision over the perineum at the posterior border of the UGS is made.11
- The flap must be long enough to provide a tension-free anastomosis to the vagina and wide enough to provide a normal-caliber introitus without compromising the blood supply of the perineal body.1
- The UGS is dissected parallel to the posterior wall of the UGS towards the posterior vaginal wall away from the rectum
- Lateral dissection should be minimized to avoid bleeding
- The posterior dissection should continue until the confluence can easily reach the introitus
- Once the posterior dissection is completed, the posterior wall of the UGS is divided in the midline as well as the posterior vaginal wall until an adequately sized vaginal opening is achieved
- The midpoint of the perineal skin flap is then sutured to the split posterior vaginal wall (Figure 5)
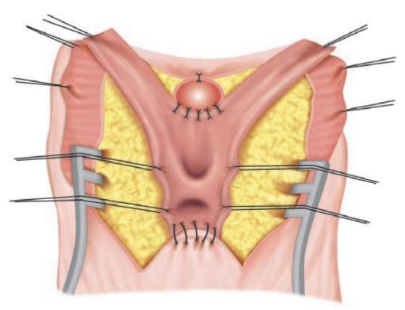
Figure 5 Diagram depicting the flap vaginoplasty. The common channel has been incised in the midline exposing the urethra and vagina. Note anchoring of the anterior apex of the UGS and the anchoring of the posterior apex to the U-shaped skin flap. The redundant common channel wall can be excised or used for additional reconstruction of the fourchette. Source: Carrasco “Surgical Techniques in Pediatric and Adolescent Urology”.6
Pull-Through Vaginoplasty
First described by: Hendren and Crawford in 196913
Indications: high confluence with short urethral length, or if extensive bladder neck mobilization is anticipated6
Position: prone
Brief description: The vagina is separated from the urogenital sinus and separately brought to the perineum while the UGS is used to create a urethra. This is ideal when there is long vaginal length with excellent elasticity.6
Steps
- A posterior perineal skin flap is created similar to the flap vaginoplasty
- The posterior and lateral walls of the UGS are dissected, extending to the posterior and lateral walls of the vagina
- The perineal body can be divided for additional exposure if necessary
- The posterior vaginal wall is then incised at its junction to the UGS to expose the confluence of the urethra and vagina
- The posterior urethral wall is separated from the anterior vaginal wall (Figure 6, A)
- Often there is no true plane between these structures
- The dissection should err to the vaginal side to minimize risk of injury to the urethra (including the sphincter1), bladder neck and ureters
- The dissection is carried as proximally as possible until the vaginal opening can be brought to the perineum with minimal tension
- The common channel defect is closed and now the common channel becomes the urethra (Figure 6, B)
- The posterior perineal flap is sutured to the vagina in a similar fashion to the flap vaginoplasty
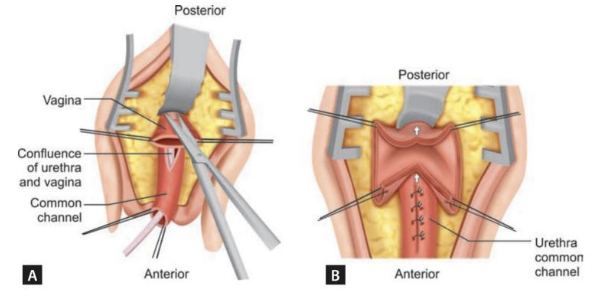
Figure 6 Diagram depicting pull-through vaginoplasty. A: The posterior vaginal wall has been incised at the level of the confluence of the urethra and vagina. B: The anterior and posterior vaginal wall are dissected proximally (arrows) to allow mobilization of the vagina towards perineum. Note the junction of the vagina to the common channel is closed making the common channel a continuation of the urethra. Source: Carrasco “Surgical Techniques in Pediatric and Adolescent Urology”.6
Anterior Sagittal Transrectal Approach
First described by: Domini et al in 199714
Indications: high confluence
Position: prone
Brief description: The high confluence is accessed posteriorly through the anterior rectal wall to separate the vagina from the urogenital sinus
Steps
- A midline perineal incision is made from the anterior anal border to the UGS opening.15
- The anterior rectal wall and anorectal sphincter are incised, exposing the posterior vaginal wall
- The posterior vaginal wall is incised as close to the urethral junction as possible
- The vagina is mobilized posterolaterally and then dissected from the urethra
- The urethral opening is closed
- The vagina is brought to the perineum, using perineal skin flaps if necessary
- The anorectal wall is closed in 2 layers
- The anorectal sphincter and perineal body are reconstructed
Laparoscopic and Robotic-Assisted Approaches
There are a few reports of laparoscopic and robotic approaches for urogenital sinus repair.16,17 The laparoscopic or robotic approach allows for dissection of the uterus and vagina away from the bladder and rectum from inside the abdomen. The vagina is then brought to the perineum.
Postoperative Care
- The postoperative care is variable, depending on the extent of surgical repair and the patient’s age.6
- A young patient undergoing a more minimal repair (e.g., flap vaginoplasty) could be discharged home the same day.
- An older patient undergoing a more extensive repair (e.g., pull-through vaginoplasty) should be admitted for observation.
- Vaginal packing can be considered in adolescent patients.
- The duration of foley catheter is 3–7 days for a flap vaginoplasty, and at least 7 days for all other repairs.
- Petroleum-based ointment should be applied to the introitus at least 4 times a day for the first few weeks to create a barrier between suture lines to prevent adherence of underwear to the wound and of tissues to each other.
Postoperative Complications
Immediate Complications
- Bleeding: can be minimized with vaginal packing in postpubertal patients.6
- Flap necrosis: rare
- Favor delayed repair to prevent local tissue fibrosis
- Wound infection: rare
- Generally managed with antibiotics
- Wound dehiscence: uncommon if anastomosis was tension free
- Can be managed conservatively to allow healing by secondary intention
- Urinary retention: rare
- If the patient is unable to void, the catheter should be replaced with a Coudé catheter. This is particularly important after pull-through vaginoplasty as the posterior wall of the UGS is delicate and prone to false passage.6
- Fistula formation: highest risk after a pull-through vaginoplasty
- Can occur anywhere in the lower urinary tract, but most common location is at the confluence of the common channel where the vagina was separated
Late Complications and Surgical Outcomes
The data on long-term outcomes following isolated urogenital sinus repair are very limited. Most data regarding vaginoplasty outcomes comes from patients with congenital adrenal hyperplasia, who tend to have more complex anatomy and require other adjunct procedures.6
- Flap vaginoplasty:
- No reports of incontinence, which aligns with the minimal dissection required
- Can have vaginal voiding due to a hypospadiac meatus
- Intravaginal hair growth from the perineal skin flap, which can interfere with sexual intercourse
- Vaginal stenosis:
- Rate ranges widely from 3% to 83%
- The rate of surgical revision also has a wide range of 25% to 86%
- Can usually be managed with vaginal dilation
-
PUM, TUM and pull-through vaginoplasty outcome data are limited
- May have higher risk of incontinence given the extent of pelvic floor dissection required.6
- Appears to have lower risk of vaginal stenosis
- ASTRA outcomes:
Key Points
- Isolated urogenital sinus is a rare congenital abnormality of the female urogenital system where the urethra and vagina fail to separate during development, forming a common channel.
- Diagnosis is primarily made on physical exam of the external genitalia of a female patient showing a single perineal orifice.
- Cystoscopy and exam under anesthesia are typically performed to better understand the anatomy. Genitogram is optional.
- Surgical reconstruction techniques depend on length of the common channel. Longer channels portend more invasive surgical techniques to mobilize urethra and vagina to the skin. Shorter channels are more common and have excellent outcomes after reconstruction.
Conclusion
Urogenital sinus is a rare congenital malformation resulting in the urethra and vagina meeting a common channel that presents as a single perineal opening. This is commonly found in patients with congenital adrenal hyperplasia. The workup and reconstruction can be varied, but in general for short, common channels the outcomes are generally favorable in the short to intermediate term. Patients should be followed through puberty to assess the vagina for adequacy prior to menarche.
Suggested Readings
- Carrasco A. Urogenital Sinus Reconstruction. Surgical Techniques in Pediatric and Adolescent Urology. New Delhi: Jaypee Brothers; 2020.
References
- Rink RC. Surgical Management of Differences of Sexual Differentiation and Cloacal and Anorectal Malformations. In: Partin AW, Dmochowski RR, Kavoussi LR, Peters CA, Wein AJ, editors. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021.
- Clavelli A. Persistent Urogenital Sinus. J Anat Soc India 2004; 59 (2): 1. DOI: 10.1016/s0003-2778(10)80034-6.
- Urogenital Sinus. The Fetal Medicine Foundation; . DOI: 10.1515/iupac.88.1463.
- Rowe CK, Merguerian PA. Developmental Abnormalities of the Genitourinary System. Avery’s Diseases of the Newborn 2023: 1260–1273. DOI: 10.1016/b978-0-323-82823-9.00076-3.
- Grosfeld JL, Coran AG. Abnormalities of the Female Genital Tract. Eur J Pediatr Surg 2006; 2: 1935–1955. DOI: 10.1016/b978-0-323-02842-4.50125-x.
- Carrasco A. Urogenital Sinus Reconstruction. Surgical Techniques in Pediatric and Adolescent Urology. New Delhi: Jaypee Brothers; 2020.
- Ding Y, Wang Y, Lyu Y, Xie H, Huang Y, Wu M, et al.. Urogenital sinus malformation: From development to management. Intractable Rare Dis Res 2023; 12 (2): 78–87. DOI: 10.5582/irdr.2023.01027.
- Tan HH, Tan SK, Shunmugan R, Zakaria R, Zahari Z. A Case of Persistent Urogenital Sinus: Pitfalls and challenges in diagnosis. Sultan Qaboos Univ Med J 2018; 17 (4): 455. DOI: 10.18295/squmj.2017.17.04.013.
- Eapen A, Chandramohan A, Simon B, Putta T, John R, Kekre A. Imaging Evaluation of Disorders of Sex Development. Journal of Gastrointestinal and Abdominal Radiology 2020; 03 (02): 181–192. DOI: 10.1055/s-0039-3402101.
- Vaginoplasty technique for female pseudohermaphrodites. Plast Reconstr Surg 1964; 34 (3): 322. DOI: 10.1097/00006534-196409000-00031.
- Jenak R, Ludwikowski B, González R. Total Urogenital Sinus Mobilization: A Modified Perineal Approach For Feminizing Genitoplasty And Urogenital Sinus Repair. J Urol 2001; 165 (6 Part 2): 2347–2349. DOI: 10.1097/00005392-200106001-00032.
- Yang J, Syed H, Baker Z, Vasquez E. Urogenital Sinus Diagnosed During Workup of Recurrent Urinary Tract Infections: A Case Report. Urology 2023; 174: 165–167. DOI: 10.1016/j.urology.2022.12.031.
- Fares AE, Marei MM, Abdullateef KS, Kaddah S, El Tagy G. Laparoscopically Assisted Vaginal Pull-Through in 7 Cases of Congenital Adrenal Hyperplasia with High Urogenital Sinus Confluence: Early Results. J Laparoendosc Adv Surg Tech A 2019; 29 (2): 256–260. DOI: 10.1089/lap.2018.0194.
- Rink RC, Cain MP. Urogenital mobilization for urogenital sinus repair. BJU Int 2008; 102 (9): 1182–1197. DOI: 10.1111/j.1464-410x.2008.08091.x.
- Hardy Hendren W, Crawford JD. Adrenogenital syndrome: The anatomy of the anomaly and its repair. Some new concepts. J Pediatr Surg 1969; 4 (1): 49–58. DOI: 10.1016/0022-3468(69)90183-3.
- Dòmini R, Rossi F, Ceccarelli PL, Castro RD. Anterior sagittal transanorectal approach to the urogenital sinus in adrenogenital syndrome: Preliminary report. J Pediatr Surg 1997; 32 (5): 714–716. DOI: 10.1016/s0022-3468(97)90012-9.
- Salle JLP, Lorenzo AJ, Jesus LE, Leslie B, AlSaid A, Macedo FN, et al.. Surgical treatment of high urogenital sinuses using the anterior sagittal transrectal approach: a useful strategy to optimize exposure and outcomes. J Urol 2012; 187 (3): 1024–1031, DOI: 10.1016/j.juro.2011.10.162.
- Leite MTC, Fachin CG, Albuquerque Maranhão RF de, Shida MEF, Martins JL. Anterior sagittal approach without splitting the rectal wall. Int J Surg Case Rep 2013; 4 (8): 723–726. DOI: 10.1016/j.ijscr.2013.05.013.
- Huen KH, Holzman SA, Davis-Dao CA, Wehbi EJ, Khoury AE. Taking “Trans-ano-rectal” out of ASTRA: An anterior sagittal approach without splitting the rectum. J Pediatr Urol 2021; 18 (1): 96–97. DOI: 10.1016/j.jpurol.2021.12.007.
- Peña A. Total urogenital mobilization–An easier way to repair cloacas. J Pediatr Surg 1997; 32 (2): 263–268. DOI: 10.1016/s0022-3468(97)90191-3.
Ultima atualização: 2024-04-05 12:50