53: Bladder and Ureteral Trauma
Este capítulo durará aproximadamente 18 minutos para leer.
Bladder Trauma
Epidemiology
The incidence of bladder rupture during childhood is low, with the condition representing about 5% of urinary tract injuries. According to the American Association for the Surgery of Trauma (AAST), the majority (92%) of bladder injuries are grade III–IV.1
Pelvic fractures are less frequently associated with bladder trauma in children (3–4% of cases) than in adults (70–80%). Another difference compared with adults is that neck lacerations are twice as frequently associated with bladder trauma in children. This fact is of great clinical importance in the diagnosis and subsequent treatment,2,3
An important factor in these injuries, especially in children, is the degree of bladder distention. A fully distended bladder can rupture even with a mild blow; however, an empty bladder is rarely damaged except by crushing or penetrating injuries. In children undergoing an intermittent catheterization (IC) program associated with bladder enlargements, the bladder is more vulnerable, and perforation is easier.
Due to the high energy necessary to damage the bladder, 60–90% of patients presenting with bladder injury have a pelvic bony fracture while 6–8% of patients with a pelvic fracture will have bladder injury. Pediatric patients are more susceptible to bladder injuries due to the childhood anatomy. A pelvic fracture with hematuria is associated with a bladder injury in 30% of cases.4
Within abdominal surgery, gynecological and obstetric procedures are the most frequent (52–61%), followed by urological interventions (12–39%) and general surgery (9–26%).
Iatrogenic bladder injuries associated with urologic surgery occur during vaginal procedures and laparoscopy. In children undergoing inguinal canal surgery, especially for intra-abdominal cryptorchidism, there may be a risk of bladder injury. During transurethral resection of tumors, the risk is generally low (1%), and most cases (88%) can be treated by drainage with a bladder catheter. Transurethral resection of the prostate is also associated with low injury rates.5
Classification
Bladder injuries are mainly of four types: intraperitoneal bladder rupture (IBR), extraperitoneal bladder rupture (EBR), bladder contusion and bladder neck avulsion. IBR occurs in 15–25% of cases. EBR is the most common type, being found in 60–90% of patients, and it is more frequently associated with pelvic fractures. Combined bladder rupture, i.e., a combination of IBR and EBR, is found in 5–12% of cases. EBR can be further classified into simple EBR, where the urinary leak is limited to the extraperitoneal pelvic region, and complex injuries, where extravasated urine infiltrates the anterior abdominal wall, the scrotum, and the perineum.6
In addition, iatrogenic lesions may arise during open lower abdominal or pelvic surgery (85% of cases) or, less frequently, during vaginal surgery, laparoscopy, or surgery on the inguinal canal. Furthermore, spontaneous lesions are possible. In this type of lesion, the bladder trauma in a healthy child is extremely rare and may go unnoticed in the face of abdominal pain, free intra-abdominal fluid, or sepsis in neonates. Perforations have been described in children with bladder diverticulum and those with bladder enlargement. The global incidence of bladder perforation in children undergoing augmentation cystoplasty is 5%, while after bladder catheterization it is 1%; 4% of cases are spontaneous.7,8,9
Extraperitoneal Bladder Injuries
In these cases, urine leakage is limited to the perivesical space. Most occur because of closed trauma and in relation to fractures of the pelvic bone frame. They can also occur in pelvic disjunctions when the bladder wall is torn by traction on the pubovesical ligaments.
Intraperitoneal Bladder Injuries
In these cases, the peritoneal surface is broken. Such injuries. Twenty-five percent occur in patients without pelvic fractures. In children, they are more frequent than extraperitoneal injuries, and in this age group they represent 77% of bladder injuries. Their incidence may have increased due to the progressive rise in use of the seat belt.
The lesion occurs more frequently in the posterior wall of the bladder and in the bladder dome, which is the place of least resistance. Another factor that favors the latter site is the lack of bone protection, which is why it is more exposed to possible traumatic agents, especially during filling,10,11
Diagnosis
Taking a clinical history is essential, and the same data must be collected as in any polytraumatized patient. In the event of pelvic fractures, the history should be directed toward potential bladder injury.
Clinical Manifestations
The clinical manifestations can be very diverse, depending on the intensity of the trauma, whether it is penetrating or not, whether the rupture is intra- or extraperitoneal, and the associated injuries. It is important to suspect such injuries in patients with pelvic fractures and to prevent them from going unnoticed, which will lead to a delay in diagnosis.
The most frequent symptoms in patients with significant bladder injuries are macroscopic hematuria and abdominal pain, and difficulty in urination may also occur.
Macroscopic Hematuria
There is a close correlation between traumatic bladder rupture, pelvic fracture, and macroscopic hematuria in 85%. Sometimes urethrorrhagia is present, which is important to consider for diagnostic maneuvers (cystography) since the urethra can be injured.
Absence of hematuria does not rule out bladder rupture: 2–10% of patients with a bladder rupture present only microhematuria or no hematuria at all (15.-17).
Abdominal Pain
This is the most common symptom after hematuria. Patients with extraperitoneal lesions tend to present diffuse abdominal pain in the hypogastrium, whereas those with intraperitoneal lesions often report pain at the level of the shoulders and in the center of the back due to accumulation of urine in the abdominal cavity and below the diaphragm. The latter patients can go for hours without having the desire to urinate due to the extravasation of urine into the abdominal cavity. With this in mind, one needs to consider the possibility of bladder rupture in patients with abdominal pain without an obvious cause, and especially in those who have undergone augmentation cystoplasty and those with bladder exstrophy, bladder diverticula, or inflammatory processes of the bladder. Delay in diagnosis can lead to serious complications.
Urinary Retention
Absence of micturition without a bladder catheter and, if necessary, other causes such as prerenal anuria or upper urinary tract injury must be ruled out.
Hematomas in the Suprapubic Region, Genitalia, or Perineum
Urine extravasation can cause swelling in the perineum, scrotum, and thighs, as well as along the abdominal wall, between the transversalis fascia and the parietal peritoneum.
Imaging Studies
Absolute indications for bladder imaging after abdominal trauma are limited to macroscopic hematuria associated with a pelvic fracture. The relative indications for imaging after blunt abdominal trauma are bladder clots, perineal hematoma, and a history of bladder enlargement. In patients with open bladder injuries, imaging studies should be obtained whenever there is suspicion that the bladder has been injured or free peritoneal fluid is observed on the initial computed tomography (CT).12,13,6
Retrograde Cystography
Retrograde cystography represents the diagnostic procedure of choice in bladder injuries and should always be performed in hemodynamically stable or stabilized patients with suspected bladder injury. CT cystography has displaced conventional cystography for this purpose, and it achieves a 95% sensitivity and 100% specificity.
Intravenous Contrast-Enhanced Ct Scan with Delayed Phase
Intravenous contrast-enhanced CT scan with delayed phase is less sensitive and specific than retrograde cystography in detecting bladder injuries.
Direct Inspection of the Intraperitoneal Bladder
Direct inspection of the intraperitoneal bladder should be performed, whenever feasible during emergency laparotomy in patients with suspected bladder injury. Intravenous dyes such as methylene blue or indigo carmine may facilitate intraoperative investigation.14,15,16
The association of pelvic fracture and macroscopic hematuria constitutes an absolute indication for immediate cystography in patients with blunt trauma. In contrast, cystography can be omitted in patients with isolated hematuria if there are no physical signs of lower urinary tract injuries.
One potentially useful imaging method that is not available in all centers, and even less so during emergencies, is urosonography or echocystography. This option has high sensitivity and specificity and avoids the drawbacks of radiation.
The study is done at the same time as assessment of other abdominal injuries and as the first diagnostic maneuver.17
Treatment
Stabilization of the patient and evaluation of the associated injuries are the priorities. Administration of antibiotics is also necessary to avoid infections that could lead to sepsis.
The surgical treatment of bladder perforations has been and remains a controversial issue.18
Extraperitoneal Injuries
Most extraperitoneal injuries can be treated by urethral catheter drainage. The important thing is to monitor the operation of the probe to avoid obstruction; if obstruction does occur, careful washing must be carried out. An efficient approach to avoid obstruction is to place a triple-lumen catheter with continuous irrigation. In children, however, this possibility does not exist, given the caliber of the triple-lumen catheters available on the market; we therefore place a urethrovesical catheter of a caliber that is appropriate to the child’s age and sufficient to allow continuous irrigation, with use of a larger suprapubic catheter for drainage. The catheter can be flushed and aspirated to avoid clogging if necessary Larger-caliber urethral catheters can lead to urethral strictures in the long term.
With this non-surgical approach, the rate of correction is 90%, and 87% of injuries have resolved at 10 days. It is to be noted that when a bone spicule is observed protruding from the bladder or located inside it, and in the case of neck lacerations, surgical intervention is mandatory.
One must not forget the association of extraperitoneal injuries with urethral injuries. To exclude the latter, a cystourethrogram should be performed. Surgical treatment is an emergency, with urethrovesical anastomosis protected by perivesical drainage and a urinary catheter.19
Intraperitoneal Injuries
Most closed intraperitoneal injuries are located in the bladder dome. They are often large and sometimes cannot be assessed radiologically.
In principle, treatment should be conservative, with placement of a urethrovesical catheter for 8–10 days. In the event of persistence of the rupture, infectious complications, or association with other serious injuries, surgery should be considered. Surgical treatment is only justified if urinary bladder drainage is inadequate or prolonged through peritoneal drainage and/or if there is no clinical improvement.
Intraperitoneal bladder injuries occur after a high degree of force, with resultant major bladder rupture. Such injuries are often associated with other abdominal injuries, requiring surgical exploration.
Surgical treatment is more commonly indicated in children because the smaller caliber of the urethral catheters used in children (referred to above) hinders effective urinary output and thus resolution of the injuries, and because there is a greater likelihood of hemodynamic instability.20,21,22
Iatrogenic Injuries
Most iatrogenic injuries can occur in the context of any surgical procedure, whether pelvic, abdominal, or vaginal. In these cases, knowledge of the injury becomes available intraoperatively, so it must be corrected at that time.
Treatment Statements
- Bladder contusion requires no specific treatment and may be observed clinically.
- Intraperitoneal bladder rupture should be managed by surgical exploration and primary repair.
- Laparoscopy may be considered for the repair of isolated intraperitoneal injuries in cases with hemodynamic stability and without other indications for laparotomy.
- In cases of severe intraperitoneal bladder rupture, during damage control procedures, urinary diversion via bladder and perivesical drainage or external ureteral stenting may be used.
- Uncomplicated blunt or penetrating extraperitoneal bladder injuries may be managed non-operatively, with urinary drainage via a urethral or suprapubic catheter in the absence of any other indication for laparotomy.
- Complex extraperitoneal bladder ruptures, i.e., bladder neck injuries, lesions associated with pelvic ring fracture, and/or vaginal or rectal injuries, should be explored and repaired.
- Surgical repair of extraperitoneal bladder rupture should be considered during laparotomy for other indications and during surgical exploration of the prevesical space for orthopedic fixations.
- In adult patients, urinary drainage by urethral catheter (without a suprapubic catheter) after surgical management of bladder injuries is mandatory. For pediatric patients, suprapubic cystostomy is recommended.6
Follow-Up
Because the purpose is to close the bladder rupture, the bladder catheter is kept in place for 9–11 days in cases of conservative treatment, while in patients who have undergone surgical correction, 7 days may be sufficient. However, before removal of the bladder catheter, cystography must be performed to check that there is no leakage. If a suprapubic catheter has been used, we first close it and, if there are no problems with urination, then remove it, also assessing whether there is postmicturition residue.22
Complications
Complications are more frequent in cases with a delay in diagnosis and therefore in treatment. The most frequent are hematoma, infections, peritonitis, and sepsis.
Urinary fistulas may occur, and their persistence requires endoscopy. Depending on the result, the treatment will be via endoscopic maneuvers or open surgery.21
Ureteral Trauma
Epidemiology and Diagnosis
Traumatic ureteral lesions are rare (less than 1%). The most common cause of ureteral injury is penetrating trauma, especially gunshot wounds; only one-third of cases are caused by blunt trauma. In blunt trauma, ureteral injuries commonly occur at the ureteropelvic junction, especially in children and in high-energy deceleration injuries. Associated organ injuries are common in patients with ureteral lesions. The clinical presentation of ureteral injuries may be subtle but isolated hematuria is a common finding.23
Injury to the ureter should be suspected in patients who have suffered high-energy blunt trauma, particularly in the presence of deceleration injuries with multisystem involvement and cases of penetrating abdominal trauma.24
Perirenal stranding or hematomas, extravasation of contrast into the perirenal space, and presence of low-density retroperitoneal fluid around the genitourinary elements at imaging are indicative of ureteral injuries. Macro- or microscopic hematuria is not a reliable sign of ureteral injury because it is absent in up to 25% of cases. A delay in diagnosis may have a negative impact on outcomes. Ultrasound plays no role in the diagnosis of ureteral injury. At delayed phase CT scan, periureteral hematoma, partial or complete obstruction of the lumen, mild distention of the ureter, hydronephrosis, delayed pyelogram, and lack of contrast in the ureter distal to the injury are all signs suggestive of ureteral injury. Urinary ascites and urinoma are considered subacute/chronic findings. A 10-min delayed phase CT scan represents a valid diagnostic tool in the diagnosis of ureteral and ureteropelvic injuries.25,26
If CT scan results are unclear, ascending urography represents the method of choice. IVU is an unreliable test (with a false negative rate of up to 60%).27
If emergency laparotomy is required, direct inspection of the ureter is indicated, and it can be associated with the use of renally excreted intravenous dye (i.e., indigo carmine or methylene blue). Single-shot IVU may be indicated intraoperatively.
Suspicion of ureteral injury is critical in any child with high-intensity abdominal trauma who has multiple concomitant injuries. Also, although traumatic ureteral lesions are rare, any injury caused by penetrating trauma should lead to suspicion of ureteral injury.
CT scan is the best method to diagnose ureteral trauma. Already in the excretory phase, it may not show passage of contrast towards the distal ureter, which may lead to suspicion of ureteral avulsion.
Although a retrograde pyelogram is probably the most accurate method to assess ureteral integrity, [it is not practical in an acute trauma setting]{:.text-decoration-underline}.
An intraoperative evaluation can also be performed by direct inspection of the ureter with the help of methylene blue injection via the urinary route or by parenteral administration of indigo carmine.28,29
Treatment
The type of treatment depends on appropriate classification of the organ damage, the general condition of the patient, the time since diagnosis, and the location of the injury.
If the ureteral injury is recognized early, the ureter must be repaired immediately (tension-free anastomosis with spatulation of both ends). If possible, the anastomotic site should also be wrapped with retroperitoneal fat or omentum. Placement of a urinary diversion (nephrostomy or ureteral stent) is recommended.
Because most ureteral injuries are diagnosed late, immediate repair during abdominal exploration is diagnosed. "Minimally invasive" treatments have become increasingly popular in this context. Percutaneous drainage of urinomas and placement of a nephrostomy tube have been shown to be useful in cases of closed and penetrating trauma to the ureter. Ureteral catheterization without open surgery has also been used successfully.
The management of ureteral contusions does not require active treatment unless there is tissue necrosis, in which case ureteral catheterization and periureteral drainage are indicated.30
Partial ureteral lacerations may be candidates for primary repair or treatment with a ureteral catheter. Management of complete lacerations and avulsions will depend on the amount of lost ureter and its location. If there is an adequate length of healthy ureter, performance of a ureteroureterostomy after wound debridement may be an option. Otherwise, reconstructive surgery is the appropriate choice, and in the case of proximal lesions, transuretero-ureterostomy, autotransplantation, and ureteral replacement with intestine or appendix appear reasonable options.
If the general condition of the patient precludes immediate repair, a transitory ureterostomy with reconstructive treatment in a second stage is an option that provides good drainage without the presence of tubes.
Avulsions of the ureteropelvic junction should be managed with a primary re-anastomosis if possible. If the ureteral length is inadequate, ureterocalicostomy is a suitable option.30
Treatment Statements
- Contusions may require ureteral stenting when urine flow is impaired.
- Partial lesions of the ureter should initially be treated conservatively with the use of a stent, with or without a diverting nephrostomy, in the absence of other indications for laparotomy.
- Partial and complete ureteral transections or avulsions unsuitable for non-operative management may be treated with primary repair plus a double J stent or ureteral re-implant into the bladder in the case of distal lesions.
- Ureteral injuries should be repaired operatively when discovered during laparotomy or in cases in which conservative management has failed.
- Ureteral stenting should be attempted in cases of partial ureteral injuries diagnosed in a delayed fashion; if this approach fails, and/or in cases of complete transection of the ureter, percutaneous nephrostomy with delayed surgical repair is indicated.
- In any ureteral repair, stent placement is strongly recommended.24
Complications
Urinary extravasation can present as a growing mass on the abdominal flank, with no signs of bleeding. Initial management should include urinary diversion, with the placement of either a double J catheter or a percutaneous nephrostomy tube. If there is already a urinoma and/or abscess, it can be drained percutaneously. Most cases evolve without the formation of ureteral stricture.31
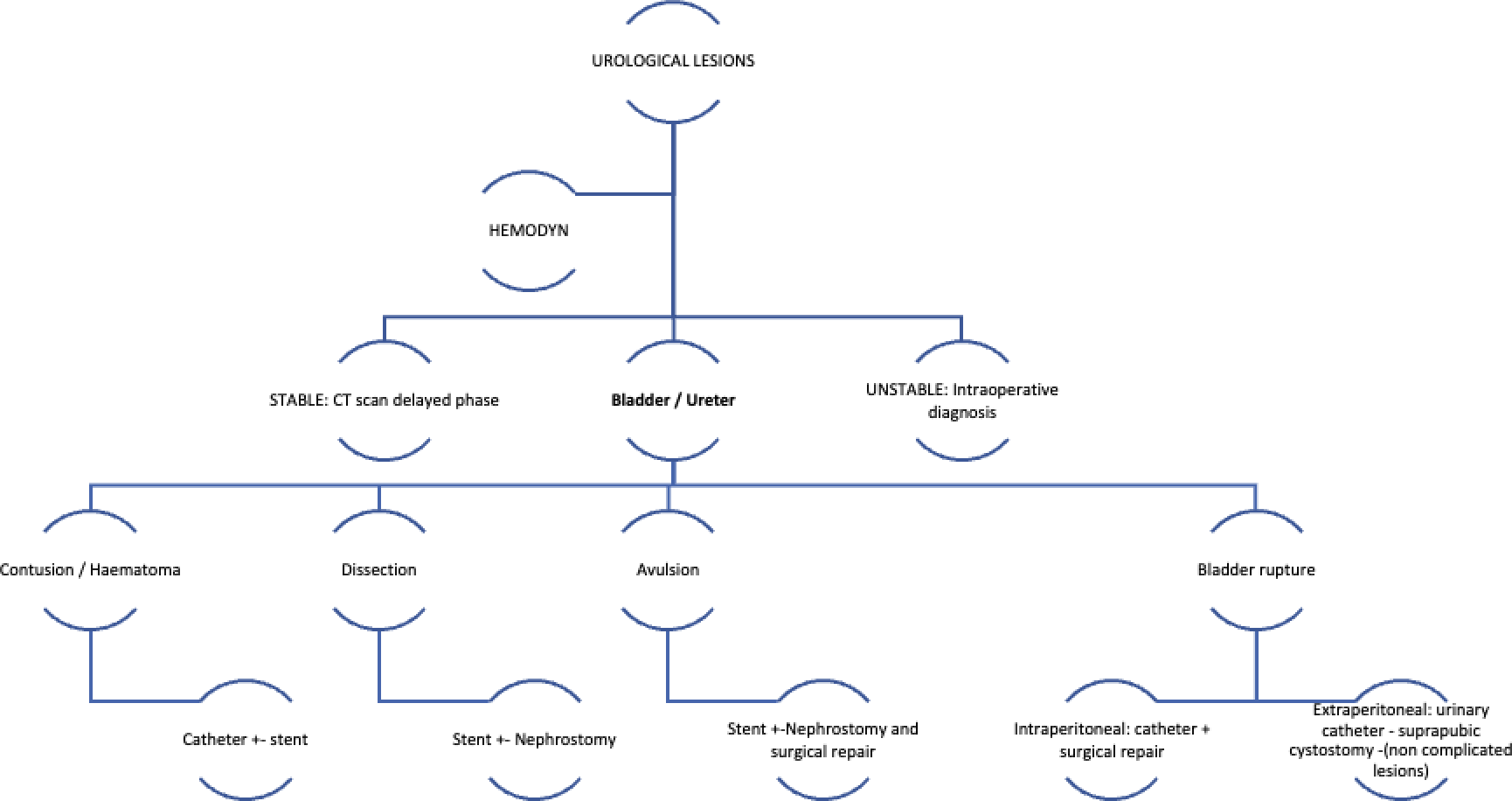
Figure 1 Types of bladder and ureteral injuries and their management6,24
Table 1 Guidelines for managing ureteral trauma.
| Recommendation | Level of evidence |
|---|---|
| Contusions may require ureteral stenting when urine flow is impaired. | 1C |
| Partial lesions of the ureter should initially be treated conservatively with the use of a stent, with or without a diverting nephrostomy in the absence of other indications for laparotomy. | 1C |
| Partial and complete ureteral transections or avulsions not suitable for non-medical management may be treated with primary repair plus a double J stent or ureteral re-implant into the bladder in the case of distal lesions. | 1C |
| Ureteral injuries should be repaired operatively when discovered during laparotomy or in cases in which conservative management has failed. | 1C |
| Ureteral stenting should be attempted in cases of partial ureteral injuries diagnosed in a delayed fashion; if this approach fails, and/or in the case of complete transection of the ureter, percutaneous nephrostomy with delayed surgical repair is indicated. | 1C |
| In any ureteral repair, stent placement is strongly recommended. | 1C |
In the absence of other indications for laparotomy, the majority of low-grade ureteral injuries (contusion or partial transection) may be managed by observation and/or ureteral stenting. If stenting is unsuccessful, a nephrostomy tube should be placed.
If ureteral injuries are suspected during a laparotomy, direct visualization of the ureter is mandatory. Whenever possible, ureteral injuries should be repaired. Otherwise, a damage control strategy should be preferred, with ligation of the damaged ureter and urinary diversion (temporary nephrostomy), followed by delayed repair.
In cases of complete transection of the ureter, surgical repair is indicated. The two main options are primary uretero-ureterostomy or ureteral re-implant with bladder psoas hitch or a Boari flap. The use of ureteral stents is recommended after all surgical repairs to reduce failures (leaks) and strictures. Distal injuries to the ureter (caudal to the iliac vessels) are usually treated by reimplantation of the ureter in the bladder (uretero-neocystostomy), as the traumatic insult may jeopardize the blood supply.
In cases of delayed diagnosis of incomplete ureteral injuries or delayed presentation, an attempt at ureteral stent placement should be done; however, retrograde stenting is often unsuccessful. In these cases, delayed surgical repair should be considered (32)
Table 2 Guidelines for managing bladder injury.
| Recommendation | Level of evidence |
|---|---|
| Bladder contusion requires no specific treatment and may be observed clinically | 1C |
| Intraperitoneal bladder rupture should be managed by surgical exploration and primary repair | 1B |
| Laparoscopy may be considered for repair of isolated intraperitoneal injuries in cases of hemodynamic stability and no other indications for laparotomy. | 2B |
| In cases of severe intraperitoneal bladder rupture, during damage control procedures, urinary diversion via bladder and perivesical drainage or external ureteral stenting may be used. | 1C |
| Uncomplicated blunt or penetrating extraperitoneal bladder injuries may be managed non-operatively, with urinary drainage via a urethral or suprapubic catheter, in the absence of other indications for laparotomy. | 1C |
| Complex extraperitoneal bladder ruptures, i.e., bladder neck injuries, lesions associated with pelvic ring fracture, and/or vaginal or rectal injuries, should be explored and repaired. | 1C |
| Surgical repair of extraperitoneal bladder rupture should be considered during laparotomy for other indications and during surgical exploration of the prevesical space for orthopedic fixations. In cases of hemodynamic instability, a urethral or suprapubic catheter may be inserted as a temporary measure and the repair of the bladder injury may be postponed. | 1C |
In general, all penetrating bladder injuries and cases of intraperitoneal bladder rupture (IBR) require surgical exploration and primary repair. Laparoscopic repair of isolated IBR is a viable option. Open surgical repair of bladder injuries is carried out in a double-layer fashion using monofilament absorbable suture. Single-layer repair is common during a laparoscopic approach.
In the absence of other indications for laparotomy, uncomplicated blunt or penetrating EBR may be managed conservatively, with clinical observation, antibiotic prophylaxis, and the insertion of a urethral catheter or suprapubic percutaneous cystostomy in cases of a concomitant urethral injury. Injury healing occurs within 10 days in more than 85% of cases. Surgical repair of EBR is indicated in complex injuries such as bladder neck injuries, injuries associated with pelvic fractures requiring internal fixation, and rectal or vaginal injuries. Furthermore, surgical repair of EBR may be considered in cases of non-resolution of urine extravasation 4 weeks after the traumatic event.
Gunshot injuries of the bladder are commonly associated with rectal injuries, which prompt fecal diversion. Commonly, these injuries are through-and-through (entry/exit site), requiring careful and complete pelvic inspection.
Urethral catheterization, whenever possible, has the same efficacy as suprapubic cystostomy; therefore routine placement of a suprapubic tube is no longer recommended. Suprapubic catheterization may be reserved for patients with associated perineal injuries. Suprapubic drainage is recommended in children after the surgical repair of bladder rupture.6
Key Points: Bladder Trauma
- The incidence of bladder rupture during childhood is low, with the condition representing about 5% of urinary tract injuries.
- Bladder injuries are mainly of four types: intraperitoneal bladder rupture (IBR), extraperitoneal bladder rupture (EBR), bladder contusion and bladder neck avulsion. IBR occurs in 15–25% of cases and EBR is the most common type, being found in 60–90% of patients, and it is more frequently associated with pelvic fractures.
- Absolute indications for bladder imaging after abdominal trauma are limited to macroscopic hematuria associated with a pelvic fracture.
- Stabilization of the patient and evaluation of the associated injuries are the priorities.
- Bladder contusion requires no specific treatment and may be observed clinically.
- Intraperitoneal bladder rupture should be managed by surgical exploration and primary repair.
- Uncomplicated blunt or penetrating extraperitoneal bladder injuries may be managed non-operatively, with urinary drainage via a urethral or suprapubic catheter in the absence of any other indication for laparotomy.
- Complex extraperitoneal bladder ruptures, i.e., bladder neck injuries, lesions associated with pelvic ring fracture, and/or vaginal or rectal injuries, should be explored and repaired.
Key Points: Ureteral Trauma
- Traumatic ureteral lesions are rare (less than 1%).
- The most common cause of ureteral injury is penetrating trauma, especially gunshot wounds; only one-third of cases are caused by blunt trauma.
- Perirenal stranding or hematomas, extravasation of contrast into the perirenal space, and presence of low-density retroperitoneal fluid around the genitourinary elements at imaging are indicative of ureteral injuries.
- CT scan is the best method to diagnose ureteral trauma. Already in the excretory phase, it may not show passage of contrast towards the distal ureter, which may lead to suspicion of ureteral avulsion.
- Contusions may require ureteral stenting when urine flow is impaired.
- Partial lesions of the ureter should initially be treated conservatively with the use of a stent, with or without a diverting nephrostomy, in the absence of other indications for laparotomy.
- Partial and complete ureteral transections or avulsions unsuitable for non-operative management may be treated with primary repair plus a double J stent or ureteral re-implant into the bladder in the case of distal lesions.
- Ureteral injuries should be repaired operatively when discovered during laparotomy or in cases in which conservative management has failed.
References
- Husman D. Traumatismo genitourinario pediátrico. In: J WA, R KL, W PA, A PC, editors. Cambell-Walsh, vol. 132. 9a ed. Carroll PR, Mcaninch JW: J Urol; 2007. DOI: 10.4067/s0370-41062000000500014.
- Djakovic N, Plas E, Piñeiro LM, Th. Lynch YM, Santucci RA, Serafetinidis E, et al.. Guía de consenso sobre los contenidos de los protocolos de ensayos clínicos. Medicina Clínica 2010; 141 (4): 161–162. DOI: 10.1016/j.medcli.2013.01.033.
- Armenakas NA, Pareek G, Fracchia JA. Iatrogenic bladder perforations: longterm followup of 65 patients. Journal of the American College of Surgeons 2004; 198 (1): 78–82. DOI: 10.1016/j.jamcollsurg.2003.08.022.
- Dobrowolski ZF, Lipczyñski W, Drewniak T, Jakubik P, Kusionowicz J. External and iatrogenic trauma of the urinary bladder: a survey in Poland. BJU International 2002; 89 (7): 755–756. DOI: 10.1046/j.1464-410x.2002.02718.x.
- Schneider RE. Genitourinary Trauma. Emergency Medicine Clinics of North America 1993; 11 (1): 137–145. DOI: 10.1016/s0733-8627(20)30663-5.
- En GJMT, M GJ, R G. "Xxiv Congress Sociedad Iberoamericana De Urología Pediátrica (Siup) ". Xxiv Congress Sociedad Iberoamericana De Urología Pediátrica (Siup) 1987: 529–530. DOI: 10.3389/978-2-88963-089-9.
- Stein RJ, Matoka DJ, Noh PH, Docimo SG. Spontaneous perforation of congenital bladder diverticulum. Urology 2005; 66 (4): 881.e5–881.e6. DOI: 10.1016/j.urology.2005.04.004.
- Crandall ML, Agarwal S, Muskat P, Ross S, Savage S, Schuster K, et al.. Application of a uniform anatomic grading system to measure disease severity in eight emergency general surgical illnesses. Journal of Trauma and Acute Care Surgery 2014; 77 (5): 705–708. DOI: 10.1097/ta.0000000000000444.
- Bakal U, Sarac M, Tartar T, Ersoz F, Kazez A. Bladder perforations in children. Nigerian Journal of Clinical Practice 2015; 18 (4): 483. DOI: 10.4103/1119-3077.151752.
- Hwang EC, Kwon DD, Kim CJ, Kang TW, Park K, Ryu SB, et al.. Eosinophilic cystitis causing spontaneous rupture of the bladder in a child Int J Urol. 2006; 13 (4): 449–450. DOI: 10.1111/j.1442-2042.2006.01320.x.
- Giutronich S, Scalabre A, Blanc T, Borzi P, Aigrain Y, O’Brien M, et al.. Spontaneous bladder rupture in non-augmented bladder exstrophy. Journal of Pediatric Urology 2016; 12 (6): 400.e1–400.e5. DOI: 10.1016/j.jpurol.2016.04.054.
- Morgan DE, Nallamala LK, Kenney PJ, Mayo MS, Rue LW. CT Cystography. American Journal of Roentgenology 2000; 174 (1): 89–95. DOI: 10.2214/ajr.174.1.1740089.
- Abou-Jaoude WA, Sugarman JM, Fallat ME, Casale AJ. Indicators of genitourinary tract injury or anomaly in cases of pediatric blunt trauma. Journal of Pediatric Surgery 1996; 31 (1): 86–90. DOI: 10.1016/s0022-3468(96)90325-5.
- Morey AF, Iverson AJ, Swan A, Harmon WJ, Spore SS, Bhayani S, et al.. Bladder Rupture after Blunt Trauma: Guidelines for Diagnostic Imaging. The Journal of Trauma: Injury, Infection, and Critical Care 2001; 51 (4): 683–686. DOI: 10.1097/00005373-200110000-00010.
- Horstman WG, McClennan BL, Heiken JP. Comparison of computed tomography and conventional cystography for detection of traumatic bladder rupture. Urologic Radiology 1991; 12 (1): 188–193. DOI: 10.1007/bf02924005.
- Morey AF, Hernandez J, McAninch JW. Reconstructive surgery for trauma of the lower urinary tract. Urologic Clinics of North America 1999; 26 (1): 49–60. DOI: 10.1016/s0094-0143(99)80006-8.
- Deck AJ, Shaves S, Talner L, Porter JR. Computerized Tomography Cystography For The Diagnosis Of Traumatic Bladder Rupture. The Journal of Urology 2000; 64 (1): 43–46. DOI: 10.1097/00005392-200007000-00011.
- Shin SS, Jeong YY, Chung TW, Yoon W, Kang HK, Kang TW, et al.. The Sentinel Clot Sign: a Useful CT Finding for the Evaluation of Intraperitoneal Bladder Rupture Following Blunt Trauma. Korean Journal of Radiology 2007; 8 (6): 492. DOI: 10.3348/kjr.2007.8.6.492.
- Karmazyn B. CT cystography for evaluation of augmented bladder perforation: be safe and know the limitations. Pediatric Radiology 2016; 46 (4): 579–579. DOI: 10.1007/s00247-015-3501-y.
- Kessler DO, Francis DL, Esernio-Jenssen D, D.. Bladder Rupture After Minor Accidental Trauma. Pediatric Emergency Care 2010; 26 (1): 43–45. DOI: 10.1097/pec.0b013e3181c8c5f2.
- Chan DPN, Abujudeh HH, Cushing GL, Novelline RA. CT Cystography with Multiplanar Reformation for Suspected Bladder Rupture: Experience in 234 Cases. American Journal of Roentgenology 2006; 187 (5): 1296–1302. DOI: 10.2214/ajr.05.0971.
- Hayes EE, Sandler CM, Corriere JN. Management of the Ruptured Bladder Secondary to Blunt Abdominal Trauma. Journal of Urology 1983; 129 (5): 946–947. DOI: 10.1016/s0022-5347(17)52472-6.
- JN C Jr, CM S. Management of the ruptured bladder: seven years of experience with 111 cases J Trauma. 1986; 26 (9): 830–833. DOI: 10.1097/00005373-198609000-00009.
- Parra RO. Laparoscopic Repair of Intraperitoneal Bladder Perforation. Journal of Urology 1994; 151 (4): 1003–1005. DOI: 10.1016/s0022-5347(17)35150-9.
- Osman Y, El-Tabey N, Mohsen T, El-Sherbiny M. Nonoperative Treatment Of Isolated Posttraumatic Intraperitoneal Bladder Rupture In Children—is It Justified? Journal of Urology 2005; 173 (3): 955–957. DOI: 10.1097/01.ju.0000152220.31603.dc.
- Bhanot A, Bhanot A. Laparoscopic Repair in Intraperitoneal Rupture of Urinary Bladder in Blunt Trauma Abdomen. Surgical Laparoscopy, Endoscopy &Amp; Percutaneous Techniques 2007; 17 (1): 58–59. DOI: 10.1097/01.sle.0000213760.55676.47.
- Tander B, Karadag CA, Erginel B, Demirel D, Bicakci U, Gunaydin M, et al.. Laparoscopic repair in children with traumatic bladder perforation. Journal of Minimal Access Surgery 2016; 12 (3): 292. DOI: 10.4103/0972-9941.169973.
- Coccolini F, Moore EE, Kluger Y, Biffl W, Leppaniemi A, Matsumura Y, et al.. Kidney and uro-trauma: WSES-AAST guidelines. World Journal of Emergency Surgery 2019; 14 (1): 1–25. DOI: 10.1186/s13017-019-0274-x.
- McAleer IM, Kaplan GW, Scherz HC, Packer MG, P.Lynch F. Genitourinary trauma in the pediatric patient. Urology 1993; 42 (5): 563–567. DOI: 10.1016/0090-4295(93)90274-e.
- Coccolini F, Moore EE, Kluger Y, Biffl W, Leppaniemi A, Matsumura Y, et al.. Kidney and uro-trauma: WSES-AAST guidelines. World Journal of Emergency Surgery 2019; 14 (1): 1–25. DOI: 10.1186/s13017-019-0274-x.
- McGahan JP, Rose J, Coates TL, Wisner DH, Newberry P. Use of ultrasonography in the patient with acute abdominal trauma. Journal of Ultrasound in Medicine 1997; 16 (10): 653–662. DOI: 10.7863/jum.1997.16.10.653.
- Mutabagani KH, Coley BD, Zumberge N, McCarthy DW, Besner GE, Caniano DA, et al.. Preliminary experience with focused abdominal sonography for trauma (FAST) in children: Is it useful? Journal of Pediatric Surgery 1999; 34 (1): 48–54. DOI: 10.1016/s0022-3468(99)90227-0.
- Buckley JC, McAninch JW. Revision of Current American Association for the Surgery of Trauma Renal Injury Grading System. Journal of Trauma: Injury, Infection &Amp; Critical Care 2011; 70 (1): 35–37. DOI: 10.1097/ta.0b013e318207ad5a.
- Buckley JC, Mcaninch JW. Pediatric Renal Injuries: Management Guidelines From A 25-year Experience. Journal of Urology 2004; 172 (2): 687–690. DOI: 10.1097/01.ju.0000129316.42953.76.
- Broghammer JA, Langenburg SE, Smith SJ, Santucci RA. Pediatric blunt renal trauma: Its conservative management and patterns of associated injuries. Urology 2006; 67 (4): 823–827. DOI: 10.1016/j.urology.2005.11.062.
- Wright JL, Nathens AB, Rivara FP, Wessells H. Renal and Extrarenal Predictors of Nephrectomy from the National Trauma Data Bank. Journal of Urology 2006; 175 (3): 970–975. DOI: 10.1016/s0022-5347(05)00347-2.
- Armenakas NA. Ureteral Trauma: Surgical Repair. Atlas of the Urologic Clinics 1998; 6 (2): 71–84. DOI: 10.1016/s1063-5777(05)70167-5.
Última actualización: 2023-02-22 15:40