16: 膀胱输尿管反流
阅读本章大约需要 19 分钟。
引言
膀胱输尿管返流(VUR)是指尿液自膀胱逆行流入输尿管,有时甚至进入肾脏。VUR 是复发性肾盂肾炎、肾瘢痕、肾功能不全和高血压的危险因素,并被认为是儿童终末期肾病的病因之一。1,2,3,4 对返流的管理主要通过预防肾盂肾炎来减少这些长期不良后果的发生。
在过去的数十年间,VUR的评估与管理经历了范式转变,临床医生应当意识到VUR管理中的争议。有证据表明,对返流进行积极治疗已改善部分儿童的结局,使与返流相关的肾病的发生率持续下降;然而,近期泌尿外科文献提示VUR的自然病程并不遵循单一的演变模式。许多存在返流的儿童无论接受诊断还是治疗都未能获益,因为其自发消退率很高且无不良影响。5,6 明确哪些儿童能够从治疗中获益,是推动膀胱输尿管返流管理进展的最大挑战。
背景、发病率和病理生理
VUR在儿童中的发生率约为1-3%,据报道,美国年龄0-21岁的新发ESRD患者中有2.3%以返流性肾病为主要诊断。以返流性肾病为主要病因的ESRD发病率在过去二十年中稳步下降。7 先前的国际研究估计患病率更高,约为10%。5,8
尽管早在公元1世纪就已有关于返流概念的解剖学记载,但直到20世纪50年代的关键性研究才首次促成了我们今天对VUR、慢性肾盂肾炎和肾瘢痕之间关联的理解。9,10
VUR可分为原发性或继发性。原发性VUR归因于在输尿管膀胱连接处穿过逼尿肌的输尿管壁内段异常偏短。在正常的连接处,膀胱充盈时壁内输尿管受到被动压迫,从而形成抗返流机制。该机制取决于壁内段的长径比以及输尿管-膀胱插入角。11
短的膀胱壁内隧道与VUR相关,且隧道长度与返流的严重程度成反比。12
当下尿路功能异常且膀胱内压升高,足以克服抗反流机制时,便会出现继发性膀胱输尿管反流,并常与膀胱出口梗阻(例如,后尿道瓣膜)或神经源性膀胱等情况相关。继发性膀胱输尿管反流也可见于没有泌尿生殖系统或神经系统解剖学异常、但存在膀胱和肠道功能障碍的儿童。13 继发性反流最常见的病因是非神经源性膀胱和肠道功能障碍,这也是发生突破性尿路感染的最重要危险因素之一。
遗传方式
原发性VUR存在明显的遗传模式,其中同卵双胞胎中多达80%、异卵双胞胎中35%在VUR的存在方面表现一致。2 已在原发性VUR患者中鉴定出多种与输尿管芽发育异常相关的多态性,尽管尚未发现单一基因占主导地位。14 非双生同胞发生返流的概率约为25%,后代发生返流的几率约为35-50%。15,16 有趣的是,在存在排尿-排便功能障碍的儿童中,这种相关性并不那么强,这很可能说明该队列中的VUR具有继发性性质。17
膀胱输尿管返流、尿路感染与肾瘢痕
VUR 的临床意义主要在于其与先天性肾发育不良的相关性,以及因反复发作的肾盂肾炎而继发发生的肾实质损伤。至少三分之一的 VUR 患者存在肾瘢痕。18,19 瘢痕的存在意味着肾脏受损区域的存在,并增加长期不良后遗症的风险。
先天性反流性肾病
在患有膀胱输尿管返流(VUR)的新生儿中,在临床尿路感染(UTI)发生之前,已检测到与高级别返流相关的瘢痕。20 这些”先天性瘢痕”被认为是由肾发生异常导致的局灶性发育不良或发育不全区域,而非肾盂肾炎后受损的正常组织。先天性肾发育不良可能与感染继发的获得性肾瘢痕难以区分。由于DMSA扫描并不在新生儿中常规实施,因此,归因于感染性损伤的肾瘢痕中有多大比例实际上源于胚胎发生异常尚不清楚。21 尽管最终病因仍不确定,它们是肾功能降低的区域,并且独立于感染相关性肾瘢痕的形成,可与显著的发病率和死亡率相关。22
肾盂肾炎与肾瘢痕
尿路感染在儿童中很常见,影响约5%的女孩,男孩约为其一半。23 据估计,5岁以下发生尿路感染的儿童中,进一步评估可发现30-40%存在膀胱输尿管返流(VUR)。24,25 肾瘢痕被认为是在受感染尿液与肾实质接触引发炎性反应时发生;其与高血压、蛋白尿和肾功能不全风险增加有关。3,26
VUR(膀胱输尿管返流)作为感染相关肾损伤的易感因素,最初在脊髓损伤患者中被认识到。手术矫治后,这些儿童肾盂肾炎和泌尿源性败血症的发作次数更少。27 进一步的研究表明,与由神经源性膀胱或排尿功能障碍导致的继发性返流儿童相比,原发性返流儿童新发肾瘢痕的发生率更低。28,29
由肾盂肾炎导致的永久性肾损伤可在99mTc-二巯基丁二酸(DMSA)显像上表现为肾瘢痕。于一项检视因尿路感染住院儿童是否存在肾损害的荟萃分析中,约有34%的肾盂肾炎患儿存在VUR,而在合并VUR且患有肾盂肾炎者中,72%有异常的DMSA显像。30
在放射性核素显像中,肾瘢痕可能在急性肾盂肾炎发作期间或不久之后即可被检出。由肾瘢痕引起的后遗症可能多年都不显现;已有报道,从首次导致肾瘢痕的肾盂肾炎到出现高血压或终末期肾病可间隔长达30–40年。27 明显的初始肾脏损伤与临床上显现的后果之间的漫长间隔,强调了对膀胱输尿管返流(VUR)患者进行长期随访的必要性。
反流分级及其他结局预测因子
由于VUR在大多数患儿中具有较高的自行消退率,但在另一些患儿中可能导致严重的临床后果,识别风险最高的患儿是VUR管理的主要目标。国际返流研究将VUR按5级分级,该分级由尿液逆行反流的程度及伴随的肾盂肾盏系统变形所界定(图1)31 较高级别与自发消退率降低以及肾瘢痕发生率增加相关。23,32
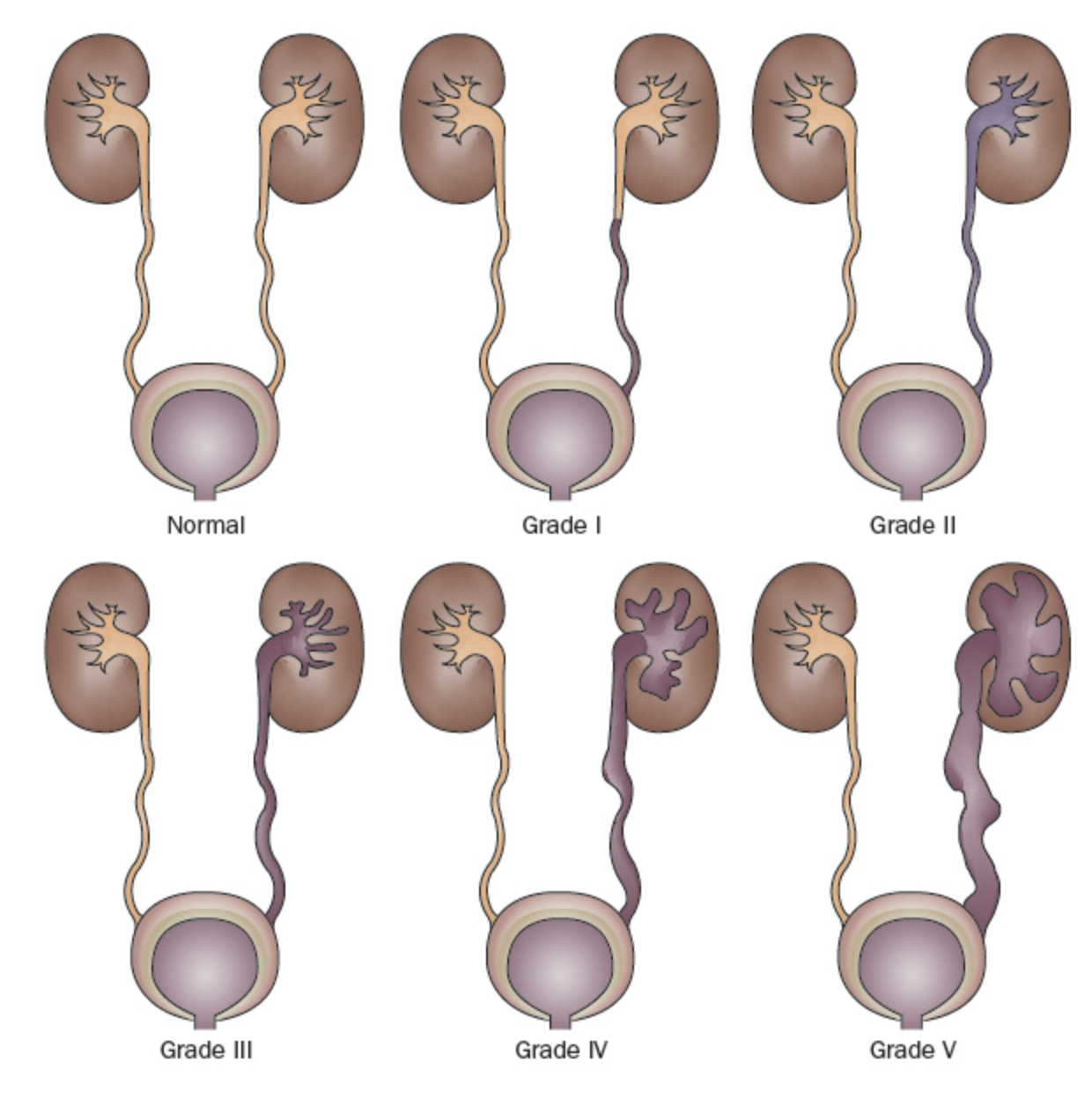
图 1 国际反流分级系统。31
- I 级: 仅返流至输尿管
- II 级: 返流进入未扩张的肾盂肾盏系统
- III 级: 肾盂肾盏系统扩张 (图 2)
- IV 级: 更广泛的扩张并伴有肾盏钝化和输尿管迂曲 (图 3)
- V 级: 肾盂肾盏系统巨大扩张并有严重的输尿管迂曲 (图 4)
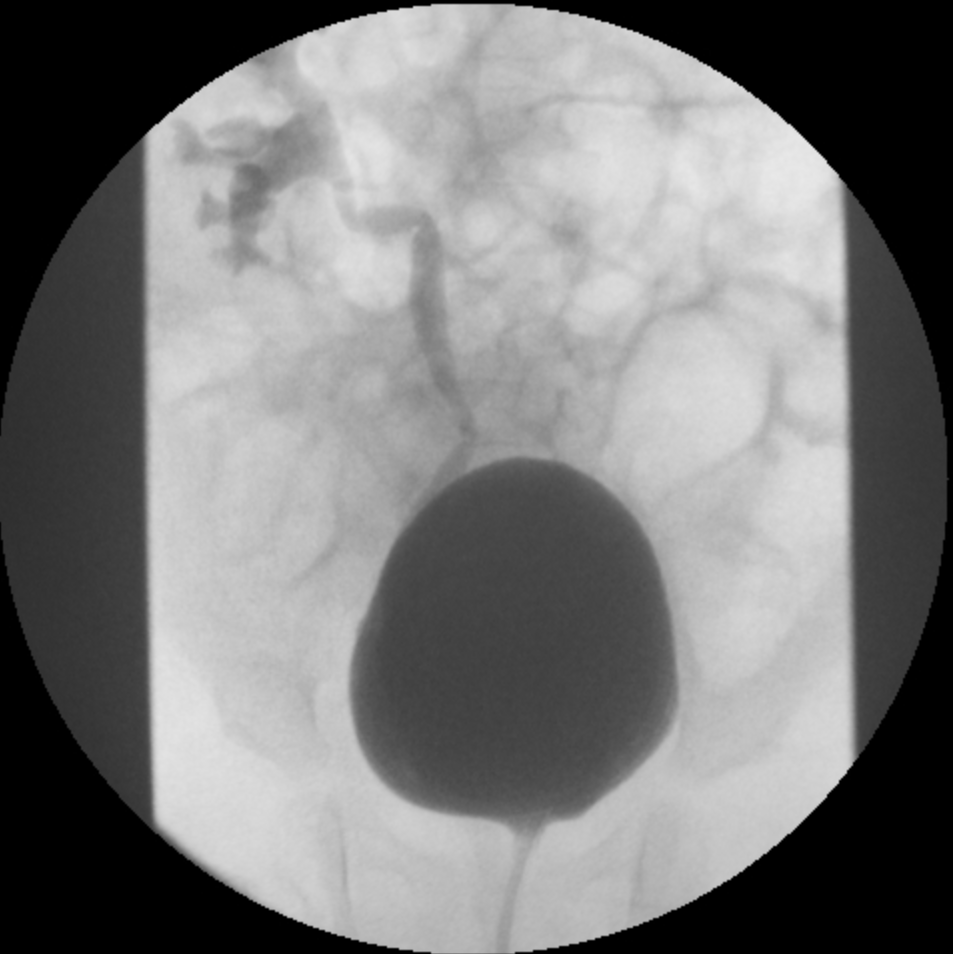
图2 III级膀胱输尿管返流
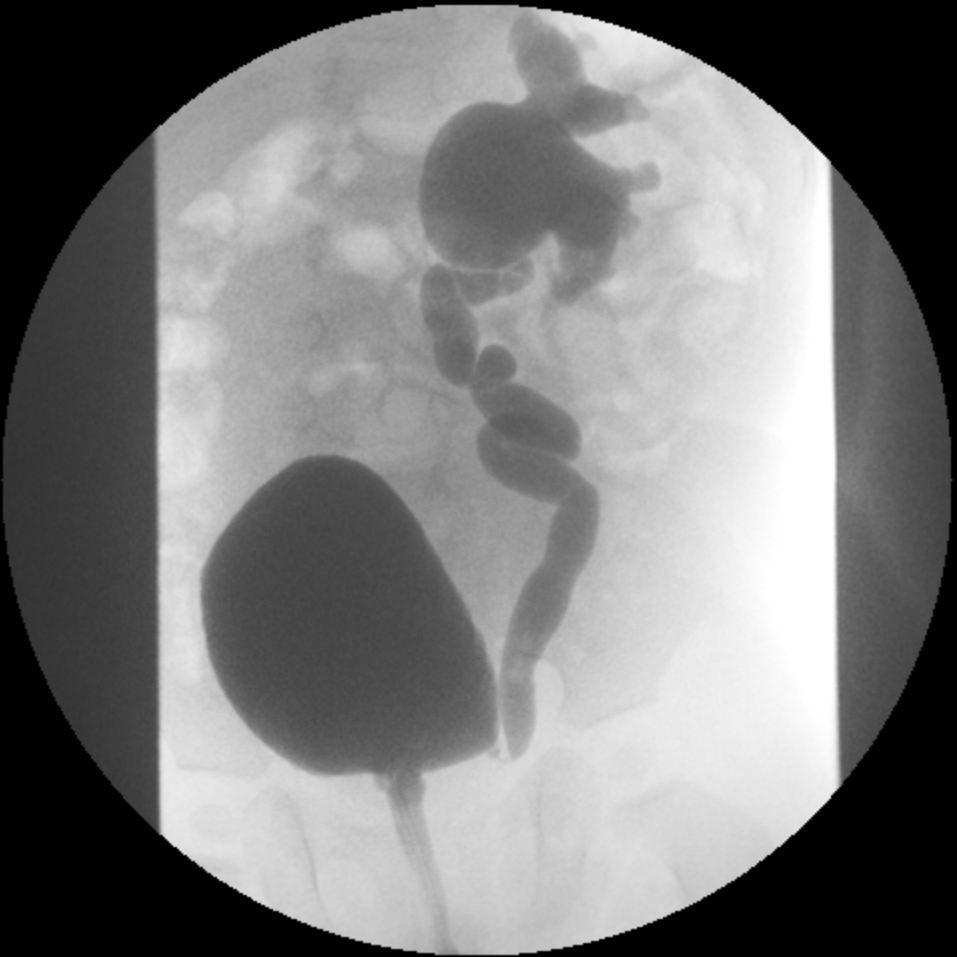
图 3 IV 级膀胱输尿管返流
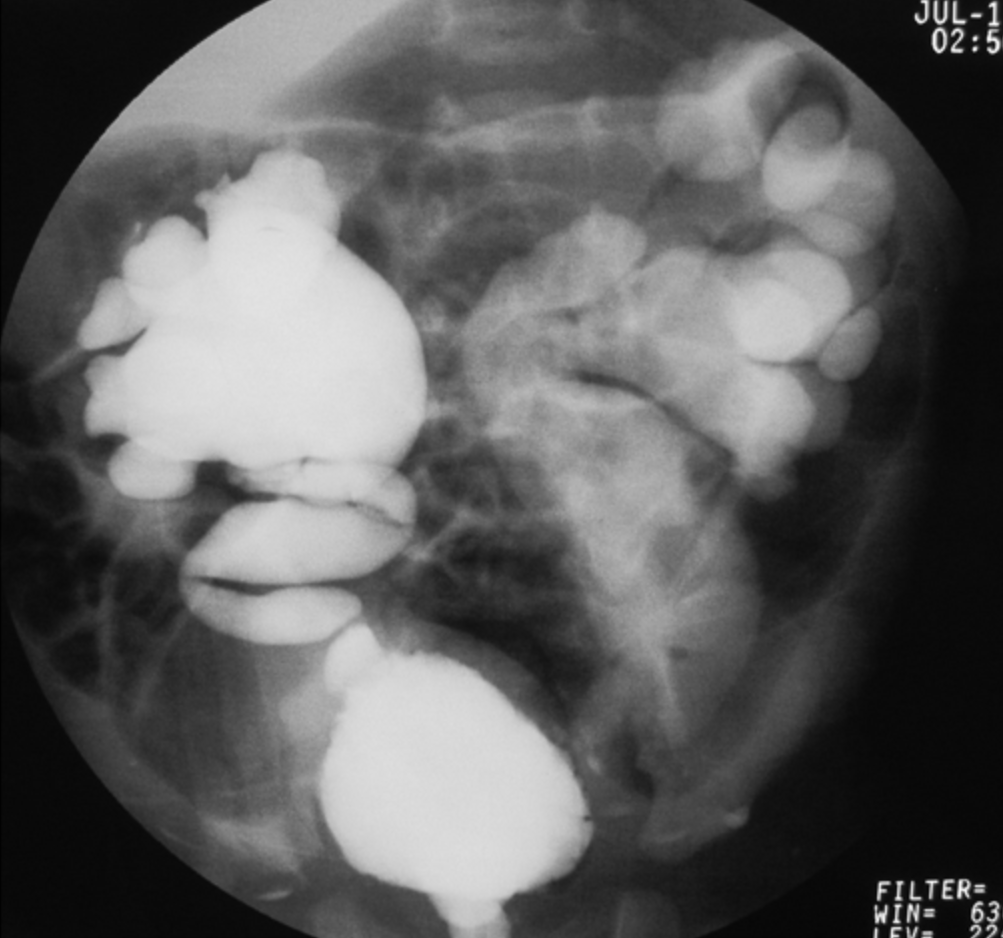
图 4 V 级 VUR
多项研究表明,肾瘢痕的患病率与返流分级之间存在直接相关性。33 在非扩张性返流中,肾瘢痕的形成较少见。22,34,35 研究显示,与I-II级返流患儿相比,III-V级返流患儿进一步发生肾实质丧失的风险更高。36,37 另有研究证实,肾瘢痕是VUR消退的负向预测因素,与返流分级无关。38 遗憾的是,国际通用的返流分级系统主观性较强,评估者间一致性较差。39,40
更近期地,已识别出更多影响反流消退和突破性尿路感染(UTI)的因素。可用于预测反流消退、肾损伤和/或突破性UTI风险的临床因素包括年龄、性别(女性性别增加风险)、包皮环切状态(包皮环切对UTI具有保护作用)、是否存在膀胱肠道功能障碍,以及既往UTI史。影像学预测因素包括侧别(单侧 vs. 双侧)、远端输尿管直径比值(相对于L1-L3椎体间距),41,42,43,44,45 反流起始时的膀胱容量(按年龄预测的膀胱容量的百分比进行标准化),46 反流起始时的膀胱压力、反流发生于充盈期或排尿期,以及是否存在肾瘢痕。38,47
对于新生儿,基于性别、VUR 分级、输尿管解剖异常以及在 VCUG 期间返流发生时相的六点膀胱输尿管返流指数已显示对 VUR 的消退、改善所需时间以及突破性尿路感染具有预测价值。48,49 同样,已创建了一个用户友好的神经网络,利用人口学信息、VUR 分级、侧别、VUR 起始时的膀胱容量、尿路感染病史、膀胱或肠道功能障碍,以及是否存在突破性发热性尿路感染来预测 VUR 消退的可能性,可在 http://pedsurocomp.lab.uiowa.edu 获取。50 考虑多个风险因素可改进对临床结局的预测,并允许对每位患者进行更为量身定制的个体化管理。
肠道与膀胱功能障碍
与具有”正常”排泄习惯的儿童相比,患有肠道或膀胱功能障碍的儿童一致显示突破性尿路感染发生率更高、肾瘢痕更多、VUR 自发消退率更低,且手术治疗后的失败率更高。1,51 在为已完成如厕训练的 VUR 儿童确定管理方案时,应将这些发现纳入考量。
反流性肾病/肾瘢痕
与没有肾瘢痕的儿童相比,存在肾瘢痕的儿童更容易发生进一步的尿路感染(UTI)并形成新的瘢痕。34,52,53 一项纳入120例患者的回顾性研究显示,与基线DMSA扫描无异常者(6%)相比,具有III–V级反流且基线DMSA扫描存在异常者发生突破性尿路感染的概率显著更高(60%);另有一项研究显示,存在肾瘢痕的患者发生突破性尿路感染的相对风险为5.1。54,55 在一项抗反流手术后平均随访12年的研究中,具有单侧肾瘢痕的儿童发生高血压的概率为11%,而具有双侧肾瘢痕者为18.5%。56 亦有研究者认为,双侧肾瘢痕儿童高血压的发生率约为20%。57 与仅有单侧瘢痕或无瘢痕的儿童相比,严重双侧肾瘢痕的儿童发生蛋白尿、慢性肾功能不全及肾衰竭的可能性显著更高。58,59 这些数据强烈提示,存在瘢痕的儿童进一步形成新增瘢痕及发生长期临床后遗症的风险升高。
诊断与评估
排尿性膀胱尿道造影与核素膀胱造影
常规且可靠检测返流的唯一检查是排尿性膀胱尿道造影(VCUG)和核素膀胱造影。VCUG 的实施方法为经尿道导管逆行向膀胱注入造影剂,并在膀胱充盈和排尿过程中获取上下尿路的透视影像。核素膀胱造影采用放射性核素显像技术进行。VCUG 作为初始检查是合适的,因为其可提供更好的解剖细节,包括旁输尿管憩室的有无、输尿管重复以及膀胱或尿道异常。它还可对返流进行更精确的分级。此外,它还能测量远端输尿管直径;该指标已被证明较分级更客观、可靠,并且在消退及临床结局方面具有相当或更高的预测价值。41,42,43,44,45
放射性核素膀胱造影的优点在于与VCUG相比可降低辐射剂量。放射性核素膀胱造影可可靠地检出各级别的膀胱输尿管返流,并且在检测间歇性VUR方面可能更为敏感(图5)60,61
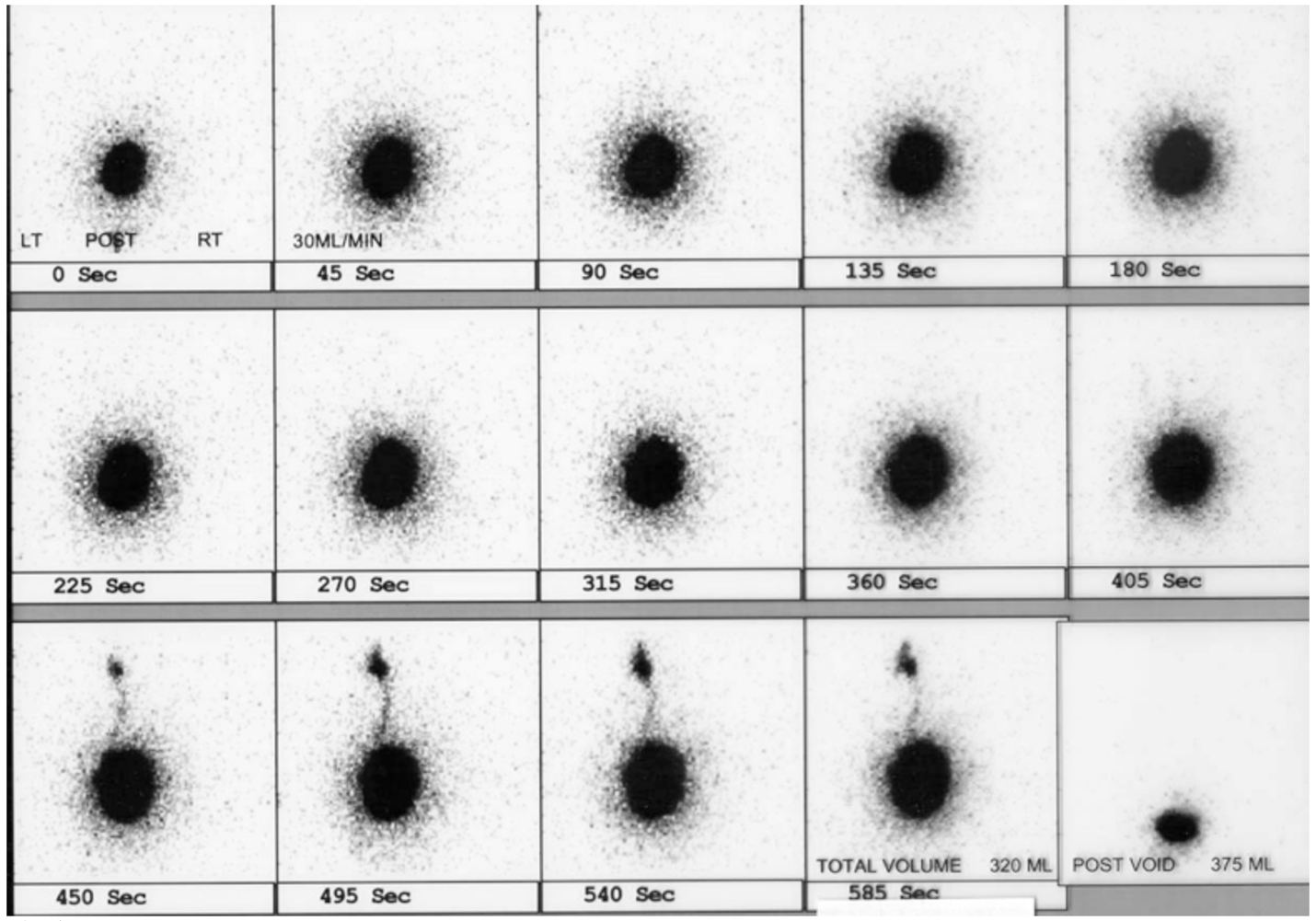
图 5 核素膀胱造影示左侧VUR
如果 VCUG 未见明显解剖异常,为了减少辐射暴露,可在随访时选择进行核素膀胱造影。尽管核素膀胱造影常被认为是一项更敏感的检查,但申请该检查的临床医生应当意识到,对于特定人群,每一种膀胱造影方法在检出膀胱输尿管返流方面都存在局限性。62
美国儿科学会泌尿外科与放射学分会于2016年制定了VCUG的标准流程,以最大限度保障患儿安全并确保获得可直接影响患儿管理的准确结果。63 主要建议包括:遵循ALARA原则,64 通过重力在高于检查台100 cm处使膀胱充盈,在排尿期获取尿道影像,进行循环检查(多次充盈循环),估算最大膀胱容量,记录发生VUR时的膀胱容量,记录排尿后残余尿量,记录膀胱或尿道异常(如膀胱憩室或后尿道瓣膜),并按照国际反流研究对返流进行分级。
除了辐射暴露外,导尿对年幼儿童来说也可能是一次创伤性的经历。为降低 VCUG 的创伤性,可采用含局部麻醉药的润滑剂、儿童生活专业人员的介入,以及清醒镇静。以往通常每年重复进行膀胱造影;然而,随着对消退时机的预测能力提高,有建议认为:对于不太可能自行消退 VUR 的儿童,应延长膀胱造影检查之间的间隔,以减少辐射暴露、创伤性检查的次数和费用。50,65,66,67
在一些中心较近期采用的一种成像方式是对比增强排尿性尿路超声造影(ceVUS),多项研究表明其在检出2级及以上VUR、检出肾内反流以及观察者间一致性方面与VCUG相当(图6)它可完全避免电离辐射,但仍需置入导尿管并进行膀胱内对比剂注入。第二代超声造影剂直到最近才在美国获得FDA批准,此前并未广泛可得。68,69 在进一步研究证明其他检测方法具有相当的敏感性和特异性之前,VCUG仍然是诊断VUR的金标准。
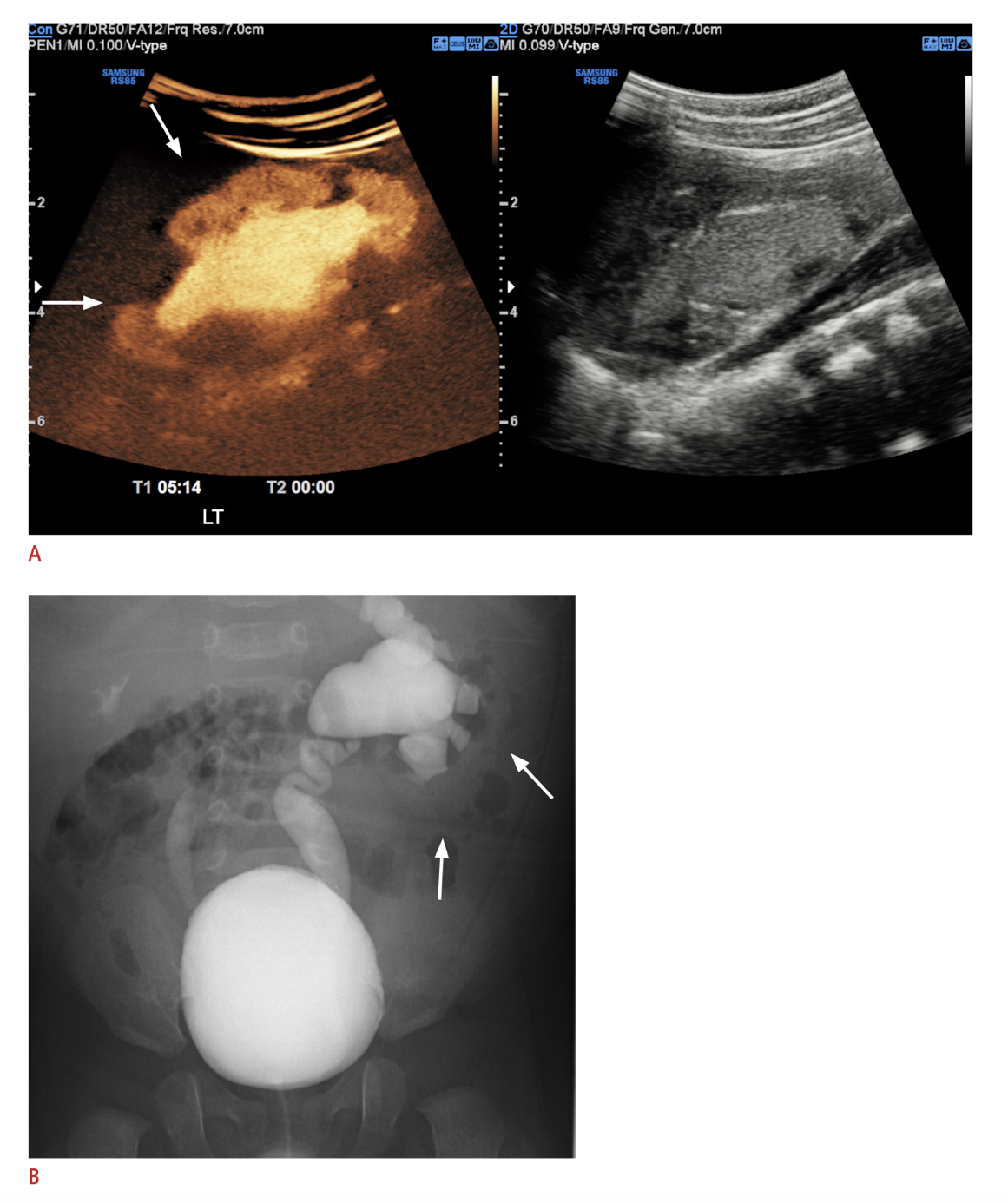
图 6 A. 左肾超声造影图像,示肾内反流;与之比较,B. VCUG显示左侧V级VUR及右侧III级VUR。图像依据 Creative Commons 署名-非商业性使用许可协议条款转载。图像转载自。版权 2021 年 韩国超声医学会。
核素闪烁显像 (DMSA, MAG3)
DMSA 肾皮质显像中,放射性药物与近端小管结合,已被发现是在检测反流性肾病方面比静脉肾盂造影(IVP)更敏感的检查。70 该显像可提供肾脏分功能信息,并且在检测急性肾盂肾炎的改变方面,其敏感性和特异性均高于CT扫描、磁共振成像或超声。71(图 7)
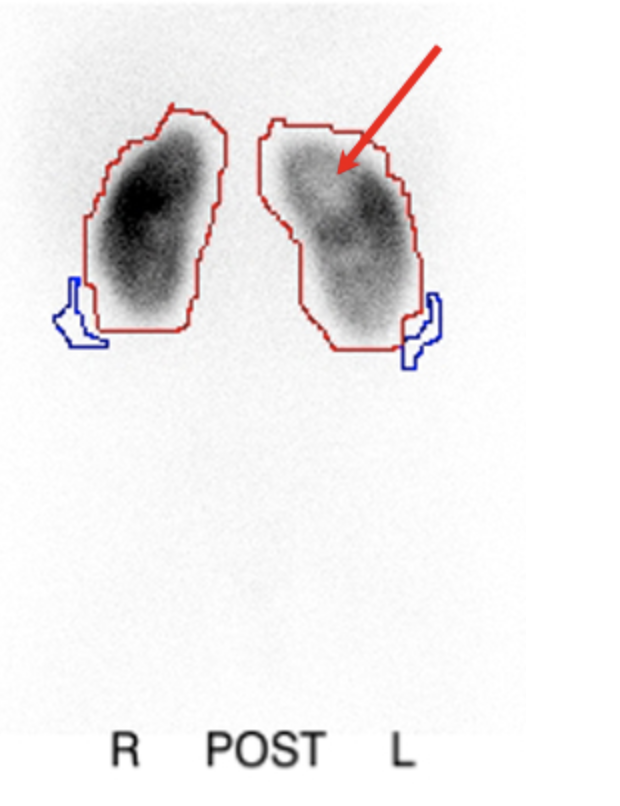
图 7 肾盂肾炎后进行的 DMSA 肾皮质显像显示左肾存在显像缺损(冷区)
肾瘢痕与更高级别返流的相关性、后续瘢痕形成的风险,以及自发消退率降低,使一些人得出结论:对发热性UTI儿童的标准初始评估应当从肾显像而非VCUG开始(”自上而下”方法)。采用这种方法,只有在肾显像异常的儿童才应进行VCUG。该方法的益处在于减少接受VCUG的儿童数量,并在更高风险人群中识别出返流;理论上,存在返流但无肾脏结构或功能异常的患者可能不会被诊断出来,但缺乏此类肾脏异常提示该返流不太可能具有临床意义。由于敏感性降低,将超声作为肾显像的替代尚未被接受。一项研究指出,DMSA上存在皮质缺损的患者中有多达25%超声检查正常,进一步提供了肾显像在评估发热性UTI儿童中的实用性数据。72
与静脉尿路造影(IVP)相比,巯基乙酰三甘氨酸(MAG3)显像在检测肾瘢痕方面的能力也有所提高。尽管许多人认为 DMSA 显像是检测肾瘢痕最敏感的检查;但据报道,MAG3 相较于 DMSA 的敏感性范围从 88% 到与 DMSA 显像相当或略优。73,74,75 MAG3 的优势包括更低的辐射暴露、成本和耗时,并且能够显示集合系统;在集合系统明显扩张者中,与 DMSA 相比这可能提高特异性。73 通常将核素显像推迟到生后 4-6 周进行,以确保肾脏发育充分,从而获得准确结果。
诊断性检查的指征
膀胱输尿管返流(VUR)的诊断通常在发生一次或多次泌尿道感染(UTI)之后作出,或在基于异常肾脏影像学所怀疑时作出。 传统上,建议对产前诊断为尿路扩张(UTD)的患者进行 VUR 筛查,因为在产前存在 UTD 的婴儿中,返流的报告发生率可高达 31%;然而,产前 UTD 与 VUR 的严重程度相关性较差。76,77,78,79 在集合系统未扩张或轻度扩张的患者中,发生 VUR 的风险可高达 25%。77,80,81 令人欣慰的是,与产前检测到的 UTD 相关的 VUR 具有较高的自发性消退发生率。81,82 评估同时存在 UTD 和 VUR 的患者是否具有较高 UTI 风险(与仅存在 UTD 而无 VUR 相比)的研究,结果相互矛盾。83,84,85,86,87,88,89,90 应根据临床意义重大的 VUR 的风险因素,审慎考虑是否进行排尿性膀胱尿道造影(VCUG)。
针对反流进行同胞筛查的效用也存在争议。17,91 在有 UTI 病史并接受筛查的同胞中,以及最终被诊断为高级别 VUR 的个体中,肾皮质异常的风险增加。92 一项使用保险理赔数据的研究未发现接受筛查与未接受筛查的同胞之间 UTI 发生率存在显著差异。93
尚需进一步证实,在无症状、经筛查的同胞中检测并处理膀胱输尿管返流(VUR)是否会显著减少不良后遗症;因此,目前对于是否对无症状同胞进行VUR筛查尚无共识。AUA《儿童原发性膀胱输尿管返流管理临床指南》建议,同胞应接受肾膀胱超声(RBUS)筛查,仅对RBUS异常者保留行排尿性膀胱尿道造影(VCUG)。94
对于有发热性UTI病史的患者,VUR评估的时机亦仍存在争议。AAP尿路感染分委员会于2011年发布并在2016年再次确认的临床指南建议:在2-24个月儿童中,若肾脏超声未见异常,则在首次发热性UTI后暂缓进行抗生素预防和VCUG。95 “儿童膀胱输尿管返流随机干预研究”(RIVUR)纳入了607名幼儿(2-72个月),他们在首次或第二次发热性或症状性UTI后被诊断为I-IV级VUR,并被随机分配至安慰剂组或抗生素预防组。甲氧苄啶/磺胺甲噁唑预防使UTI发生率降低了50%,但两组在肾瘢痕方面无显著差异,尽管该研究并未以评估肾瘢痕为主要统计效能设计。96 对RIVUR试验及另一项多中心前瞻性试验(CUTIE)的事后分析显示,第一次发热性UTI后肾瘢痕的发生率为2.8%,两次发热性UTI后为25.7%,三次或以上为28.6%,这进一步支持在初次发热性UTI后进行VUR筛查的价值。97
临床管理
对于患有 VUR 的儿童,没有普遍适用的最佳管理方案。如前所述,多种解剖与生理变量会影响 VUR 自行消退的可能性以及发热性尿路感染(UTI)的风险;同时还必须考虑患者及家庭偏好、用药依从性、社会情况以及尿路感染发生率的风险等外在因素。牢记在权衡多种影响结局的内在与外在因素后,VUR 的管理应针对每个患儿进行个体化,我们将在下文讨论各种治疗选择。
非手术治疗
每日给予低剂量(~ ¼ 治疗剂量)抗生素的做法基于如下认识:原发性VUR具有很高的自行消退率(即使在特定人群中的重度VUR亦然),而出生后反流相关的肾瘢痕似乎仅发生于尿液受感染的情况下,尤其在肾极部位,那里肾内集合系统更可能呈复合肾盏。98 因此,在反流自行消退之前维持尿液无菌,或可避免手术相关的发病率以及肾瘢痕。多项随机研究尝试评估对VUR患儿进行抗生素预防的疗效及不良反应。4,99 总体而言,这些研究未能显示接受抗生素预防的VUR患儿急性肾盂肾炎或肾瘢痕的显著减少。有些研究甚至报告,使用抗生素的患儿UTI增加,同时由耐药细菌导致的UTI也增加。4,99,100 通过亚组分析,另一些研究发现,较小年龄和反流分度升高是复发性发热性UTI的危险因素。99,101 多中心RIVUR试验证实,与安慰剂相比,抗生素预防可使UTI复发减少50%,但对肾瘢痕发生率无影响。102
许多人质疑抗生素预防的必要性,认为在部分个体中,在未使用预防性抗生素的情况下发生肾盂肾炎和肾损伤的可能性很小。103,104,105,106 有过一次尿路感染病史的儿童中有30%至50%会发生复发性感染,并且由于返流的诊断常常是在尿路感染之后做出,这使得许多人错误地认为感染是由返流引起的。然而,一般而言,除非分级较高,否则它并不会显著增加尿路感染的风险。104,107 更常见的是,尿路感染源于以下易感因素:既往尿路感染史、女性性别、便秘、排尿不频、膀胱排空不全或免疫功能受损。多项研究现已表明,对于正在接受抗生素预防且无突破性感染或肾损伤证据的儿童,可以在停止抗生素预防且不纠正VUR的情况下予以安全观察。103,104 尤其是在肠膀胱功能障碍已得到优化管理之后。108
总体而言,每日预防性使用抗生素似乎安全且耐受性良好,但确实会带来成本和潜在风险。其与出现对甲氧苄啶-磺胺甲噁唑耐药的大肠杆菌风险增加24倍相关。109 其他研究也证实,在接受预防性抗生素治疗的儿童中,会出现耐药率较高的其他细菌。110 除耐药性外,人们还担心长期使用抗生素对肠道和尿路微生物群以及生长发育的潜在不良影响。111,112,113,114 此外,还应考虑用药依从性。2010年的一项研究显示,仅完成处方取药的依从率只有40%,这提示许多被安排进行抗生素预防的患者从未取药。115
识别并治疗膀胱功能障碍在对VUR的保守治疗中发挥着重要作用,无论是单独实施还是联合预防性抗生素治疗。目前已认识到,继发性VUR更宜通过处理下尿路功能障碍来进行管理。116
几项大型前瞻性研究尝试评估手术干预与抗生素预防的疗效。这些研究普遍显示,在肾功能或肾脏生长、既有瘢痕的进展或新瘢痕的形成,以及尿路感染(UTI)方面并无显著差异。23,36,107,117,118 然而,包括发热性尿路感染在内的肾盂肾炎相关症状在药物治疗组往往更为常见。18,105,119 总体而言,最终接受手术干预的儿童往往在更早年龄出现肾瘢痕,但随访时间延长后,与手术治疗相比,接受抗生素治疗者在新发肾瘢痕方面总体并无显著差异。24,120 这些观察提示,抗反流手术对部分患者的潜在获益可能在于减少肾盂肾炎;然而,亦有研究者提出,一旦出现肾瘢痕,疾病倾向于按其自然病程发展,手术治疗获益甚微。27,121 一项综述认为,需要进行9例输尿管再植术才能预防1例发热性尿路感染,而发生肾损害的儿童数量并未减少,24 这再次强调有必要更好地界定哪些膀胱输尿管反流(VUR)患儿可能从干预中受益。一般而言,手术干预通常保留用于以下患儿:在抗生素预防期间仍出现突破性尿路感染者、肾功能恶化者,或在其他因素权衡下较每日抗生素给药更适合采取根治性干预者。
手术治疗
内镜治疗
自FDA于2001年批准将右旋糖酐/透明质酸共聚物(Dx/HA)(Deflux®,Q-Med,瑞典乌普萨拉)用于治疗原发性膀胱输尿管返流(VUR)以来,临床医师越来越多地采用内镜注射作为长期抗生素治疗的替代方案。122 Dx/HA 是美国唯一一种获得FDA批准、可商业获得的用于治疗返流的注射制剂。它是一种将右旋糖酐微球分散于透明质酸凝胶中的合成混合物,通过在输尿管口区域采用不同的技术进行注射。右旋糖酐颗粒的粒径可防止经淋巴系统迁移。123
VUR 的内镜矫治是一种微创、可在门诊完成且并发症风险低的手术。尽管这似乎是一项简单的手术,多项研究已表明其存在学习曲线,随着经验的增加可获得更好的结果。124,125,126 与内镜矫治成功相关的其他因素包括较低的返流分级、更小的 UDR、无肠膀胱功能障碍、注射更大量的 Dx/HA、对注射后隆起形态的视觉评估,以及手术技术。126,127,128,129 有关手术技术的研究表明,双重水扩张植入技术(HIT)较包括 STING 技术在内的其他技术具有更高的成功率,其成功率接近输尿管再植术。130
在短期内,以Dx/HA治疗的单个输尿管的VUR消退率为59%至95%。126,131 若患者因持续性VUR而接受第二次注射,成功率会提高,但第三次注射很少能够治愈。122,124,132 随访>5 年的患者的长期结局显示,VUR消退率为59-100%,且显著受VUR程度影响;注射后发热性UTI的发生率为4-25%。130 为确认VUR消退而常规行VCUG具有争议,一些人认为并非必需,除非患者被认为复发高风险(高分级VUR、注射后出现发热性UTI、年龄 < 2 岁),或出于家属或术者偏好。133 也有人主张,只有在超声未能显示隆起时才选择性进行VCUG。术后应进行超声检查以排除输尿管梗阻。134
除治疗失败之外,由于异物反应继发的植入物钙化最近被报道为另一种潜在的长期问题。注射形成的隆起钙化并非 Dx/HA 所特有,已在多种内镜注射剂中有所描述。135,136 这种钙化可能与输尿管结石相混淆,医护人员必须对这种情况保持高度警惕,以避免不必要的诊断检查和手术干预。137 Dx/HA 后发生输尿管梗阻的报道较少(< 1%),既可在术后不久出现,也有最迟至术后五年的报道,这强调了 Deflux 后持续进行影像学随访的重要性。梗阻可以无症状,也可表现为肾绞痛或尿路感染。138,139 梗阻通常需要切除受累段并行输尿管再植术。139,140,141
输尿管再植术
膀胱输尿管反流的外科治疗在过去五十年间不断演变。开放术式通常采用下腹部横向切口,位于皮肤皱褶处,遗留一条不显眼的小瘢痕。已应用多种输尿管再植术式;其主要差异在于经膀胱内 (图 8) 与膀胱外途径。目前尚无明确证据表明任何特定术式更优,23 术式的选择通常由手术医师酌情,并根据患儿的具体情况个体化决定。
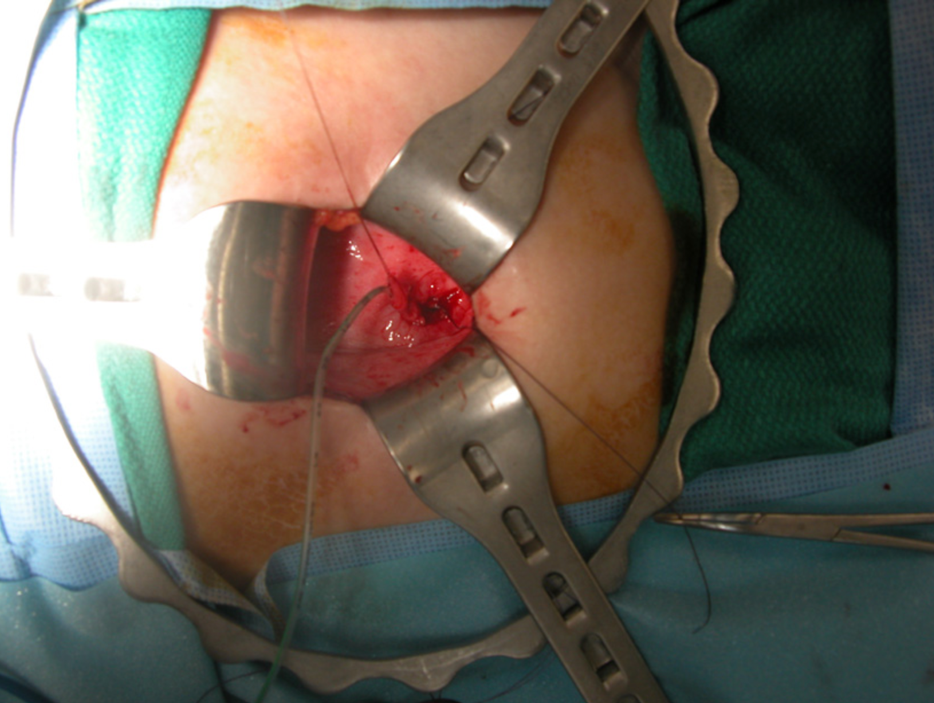
图 8 膀胱内输尿管再植术
镇痛和手术技术的进步,以及认识到针对原发性VUR行输尿管再植术的儿童很少需要输尿管支架或长期膀胱引流,使住院时间缩短并降低了手术的并发症发生率。142 数个系列报道,膀胱内途径和膀胱外途径的输尿管再植术可作为日间手术完成。143,144,145 多个系列的结果显示,开放性输尿管再植术的成功率超过95%,对于低级别返流则接近100%。146,147,148 该类手术仍存在麻醉风险和包括输尿管梗阻、持续性返流、感染及出血在内的潜在并发症。23 输尿管再植术的一般原则包括:尽量减少对输尿管的操作,切除膀胱内段输尿管,建立长度至少为输尿管腔直径5倍的隧道,并形成无张力吻合。对于粗大输尿管,为获得足够的膀胱内隧道,可能需要通过切除或折叠缝合进行整形。
近年来,机器人辅助腹腔镜膀胱外输尿管再植术的应用日益增多,据报道其益处包括减轻疼痛和缩短术后住院时间。149 一项纳入260例患者的多中心研究显示,88%的患者影像学上VUR消失,总体并发症发生率为9.6%,双侧再植术后尿潴留发生率为4%。150 一项全国性数据分析显示,与开放手术相比,并发症发生率更高(13% vs. 4.5%),且费用增加。151 尽管在一些中心仍开展机器人输尿管再植术,但开放手术的使用仍然最为普遍。152
对于考虑进行外科干预的患者,择期手术的时机仍存在争议。多数评估膀胱输尿管返流(VUR)自发缓解率的研究随访了患者5年。尽管这一终点推测是基于这样一个事实:在5岁以后发生de novo 反流性肾病的可能性下降,153许多临床医生和家属据此推断:在此时点仍未自行缓解返流的儿童应接受矫治手术。然而,对于无感染的儿童,手术时机往往可以推迟;已有关于青春期后儿童和成人行输尿管再植术的报道,鉴于成人与儿童体型差异对手术技术进行了相应调整,但总体结局良好。154
个体化管理
尽管 VUR 本身可以被简单地定义,但更为详尽的研究证实,返流并非单一疾病,其严重程度和影响存在广泛差异。关于返流的许多问题仍然未知;然而,很明显,对许多患者而言,无论是进行根治性治疗,甚至仅仅是对 VUR 作出确诊,其临床获益都存疑。目前,治疗相关的决策基于医师和家长对风险与获益的评估。尽管传统上是否选择手术主要取决于返流分级,但真正的知情决策必须综合考虑多种变量,例如患儿年龄、性别、尿路感染(UTI)史、肾功能状况、自发消退的可能性及时间,以及后续发生发热性尿路感染的风险。已经界定了多个与儿童返流自发消退几率相关的预后因素。38,47,50,65 还必须将患儿的社会情况和父母的偏好,以及对保守管理或术后护理的依从意愿,纳入考量。
在考虑多种预后变量(如年龄、性别、VUR 分级、输尿管直径比值(UDR)、返流起始时的膀胱容量、是否存在排尿功能障碍、尿路感染(UTIs)史、是否存在肾瘢痕、侧别和重复畸形)的情况下,尝试确定某一患儿 VUR 自发消退的可能性及其时间点,极其复杂。为此,一个整合了其中许多预测因素、且易于使用的神经网络可在 http://pedsurocomp.lab.uiowa.edu 使用(图 9)155
图 9 整合VUR消退预测因素的神经网络
该模型的应用和准确性已在一组日本儿童中得到国际验证。66 对于已接受肾脏显像的儿童,生成了第二个计算机模型,将额外的肾脏显像数据纳入其中以提高预后预测的准确性,并可在同一网站获取(http://pedsurocomp.lab.uiowa.edu).50
未来方向
尽管关于自发性VUR消退的可能性与时间的判断更为准确,从而允许做出更好的管理决策,但仍需更多数据。还需进一步研究以界定个体患儿随后发生肾盂肾炎、肾脏损害以及最终临床后遗影响的风险。持续从大型、多机构的前瞻性注册中收集数据,可使我们更好地理解VUR的自然史。此外,用于检测具有临床意义的膀胱输尿管返流的生物标志物,可能有助于我们更好地确定哪些患儿最能从积极治疗中获益。
要点
- 虽然国际膀胱输尿管返流(VUR)分级系统对VUR的自行消退及肾瘢痕的存在具有预测价值,但评估者间一致性较差。除分级外,更客观的影像学指标(如远端输尿管直径比值以及VUR起始时的膀胱容量)可用于预测自行消退以及突破性尿路感染的风险。
- 多种被证明可预测VUR临床结局的临床与影像学因素,被以多种组合用于风险计算器和用户友好的神经网络(如 http://pedsurocomp.lab.uiowa.edu),以实现更准确的个体化风险评估,从而更好地管理患者。
- 合并VUR相关肾瘢痕的儿童更易发生高血压、蛋白尿和慢性肾病(CKD),并应贯穿至成年期进行血压、肾功能检查及尿蛋白的常规监测。
- 仅因存在产前尿路扩张而进行VCUG往往临床意义不大;建议与家长采取共同决策的方式,结合基于其他临床与超声因素(即肾积水严重程度、是否存在输尿管扩张)的尿路感染风险,以决定儿童是否应接受VCUG。
- 充分控制肠膀胱功能障碍在膀胱输尿管返流的保守治疗中起关键作用,无论是否使用抗生素预防,在某些情况下甚至可免除手术干预的需要。
- 除了导致抗生素耐药菌的产生外,长期抗生素预防还可能具有长期副作用,包括对正常肠道和尿路微生物组的不良影响,进而影响儿童的生长发育。
参考文献
- Mathews R, Carpenter M, Chesney R. Controversies in the management of vesicoureteral reflux: the rationale for the RIVUR study. J Pediatr Urol 2009; 5 (5): 336–341. DOI: 10.1016/J.JPUROL.2009.05.010.
- Kaefer M, Curran M, Treves ST. Sibling vesicoureteral reflux in multiple gestation births. Pediatrics 2000; 105 (4 Pt 1): 800–804. DOI: 10.1542/PEDS.105.4.800.
- Smellie JM, Poulton A, Prescod NP. Retrospective study of children with renal scarring associated with reflux and urinary infection. 1994; 308 (6938): 1193–1196. DOI: 10.1136/bmj.308.6938.1193.
- Garin EH, Olavarria F, Nieto VG. Clinical significance of primary vesicoureteral reflux and urinary antibiotic prophylaxis after acute pyelonephritis: a multicenter, randomized, controlled study. Pediatrics 2006; 117 (3): 626–632. DOI: 10.1542/PEDS.2005-1362.
- Cooper CS, Austin JC. Vesicoureteral reflux: who benefits from surgery? Urol Clin North Am 2004; 31 (3): 535–541. DOI: 10.1016/j.ucl.2004.04.006.
- Mattoo TK. Vesicoureteral reflux and reflux nephropathy. Adv Chronic Kidney Dis 2011; 18 (5): 348–354. DOI: 10.1053/j.ackd.2011.07.006.
- Cornwell LB, Riddell JV, Mason MD. New-onset ESRD secondary to reflux nephropathy has decreased in incidence in the United States. J Pediatr Urol 2020; 16 (5). DOI: 10.1016/j.jpurol.2020.06.023.
- Zhang Y, Bailey RR. A long term follow up of adults with reflux nephropathy. N Z Med J 1995; 108 (998): 7761049.
- Hutch JA. Vesico-ureteral reflux in the paraplegic: cause and correction. J Urol 1952; 68 (2): 457–469. DOI: 10.1016/s0022-5347(05)65331-1.
- Hodson CJ. The radiological diagnosis of pyelonephritis. Proc R Soc Med 1959; 52 (8): 669–672.
- Kalayeh K, Fowlkes JB, Schultz WW. Ureterovesical junction deformation during urine storage in the bladder and the effect on vesicoureteral reflux. Journal of Biomechanics 2020. DOI: 10.1016/J.JBIOMECH.2020.110123.
- Paquin AJ. Ureterovesical anastomosis: the description and evaluation of a technique. J Urol 1959; 82 (5): 573–583. DOI: 10.1016/S0022-5347(17)65934-2.
- Koff SA. Relationship between dysfunctional voiding and reflux. J Urol 1992. DOI: 10.1016/s0022-5347(17)37007-6.
- AM E, K D, E R. Genes in the ureteric budding pathway: association study on vesico-ureteral reflux patients. PLoS ONE 2012; 7 (4). DOI: 10.1371/journal.pone.0031327.
- Noe HN. The long-term results of prospective sibling reflux screening. J Urol 1992. DOI: 10.1016/s0022-5347(17)37017-9.
- Wan J, Greenfield SP, Ng M. Sibling reflux: a dual center retrospective study. J Urol 1996; 156 (2 Pt 2): 8683758. DOI: 10.1016/s0022-5347(01)65782-3.
- Noe HN. The relationship of sibling reflux to index patient dysfunctional voiding. J Urol 1988; 140 (1): 3379674. DOI: 10.1016/s0022-5347(17)41502-3.
- Weiss R, Duckett J, Spitzer A. Results of a randomized clinical trial of medical versus surgical management of infants and children with grades III and IV primary vesicoureteral reflux (United States. The International Reflux Study in Children J Urol 1992. DOI: 10.1016/s0022-5347(17)36998-7.
- Smellie JM. Reflections on 30 years of treating children with urinary tract infections. J Urol 1991; 146 (2 ( Pt 2): 10 1016 0022–5347 17 37889–37888. DOI: 10.1016/s0022-5347(17)37889-8.
- Nguyen HT, Bauer SB, Peters CA. 99m Technetium dimercapto-succinic acid renal scintigraphy abnormalities in infants with sterile high grade vesicoureteral reflux. J Urol 2000; 164 (5): 10 1016 0022–5347 05 67081–67084. DOI: 10.1097/00005392-200011000-00076.
- Patterson LT, Strife CF. Acquired versus congenital renal scarring after childhood urinary tract infection. J Pediatr 2000; 136 (1): 2–4. DOI: 10.1016/s0022-3476(00)90038-6.
- Bailey RR, Lynn KL, Smith AH. Long-term followup of infants with gross vesicoureteral reflux. J Urol 1992. DOI: 10.1016/s0022-5347(17)37010-6.
- Elder JS, Peters CA, Arant BS Jr.. Pediatric Vesicoureteral Reflux Guidelines Panel summary report on the management of primary vesicoureteral reflux in children. J Urol 1997; 157 (5): 9112544. DOI: 10.1097/00005392-199705000-00093.
- Hodson EM, Wheeler DM, Vimalchandra D. Interventions for primary vesicoureteric reflux. Cochrane Database Syst Rev 2007 (3). DOI: 10.1002/14651858.CD001532.pub3.
- Baker R, Maxted W, Maylath J. Relation of age, sex, and infection to reflux: Data indicating high spontaneous cure rate in pediatric patients. J Urol 1966; 95 (1): 10 1016 0022–5347 17 63403–63407. DOI: 10.1016/s0022-5347(17)63403-7.
- Ransley PG, Risdon RA. Reflux nephropathy: effects of antimicrobial therapy on the evolution of the early pyelonephritic scar. Kidney International 1981; 20 (6): 733–742. DOI: 10.1038/KI.1981.204.
- Winberg J. Management of primary vesico-ureteric reflux in children\–operation ineffective in preventing progressive renal damage. Infection 1994; 22 Suppl 1:S4-7. DOI: 10.1007/bf01716025.
- Sukamoto E, Itoh K, Morita K. Reappraisal of Tc-99m DMSA scintigraphy for follow up in children with vesicoureteral reflux. Ann Nucl Med 1999; 13 (6): 401–406. DOI: 10.1007/bf03164934.
- Naseer S SR, G.F.. New renal scars in children with urinary tract infections, vesicoureteral reflux and voiding dysfunction: a prospective evaluation. J Urol 1997; 158 (2): 9224361. DOI: 10.1016/s0022-5347(01)64552-x.
- Gordon I, Barkovics M, Pindoria S. Primary vesicoureteric reflux as a predictor of renal damage in children hospitalized with urinary tract infection: a systematic review and meta-analysis. J Am Soc Nephrol 2003; 14 (3): 739–744. DOI: 10.1097/01.asn.0000053416.93518.63.
- Lebowitz RL, Olbing H, Parkkulainen KV. International system of radiographic grading of vesicoureteric reflux. International Reflux Study in Children Pediatr Radiol 1985; 15 (2): 105–109. DOI: 10.1007/bf02388714.
- Schwab CW Jr., Wu HY, Selman H. Spontaneous resolution of vesicoureteral reflux: a 15-year perspective. J Urol 2002; 168 (6): 2594–2599. DOI: 10.1016/S0022-5347(05)64225-5.
- Hoberman A, Charron M, Hickey RW. Imaging Studies after a First Febrile Urinary Tract Infection in Young Children. New Engl J Med 2003; 348 (3): 195–202. DOI: 10.1056/NEJMoa021698.
- Ylinen E, Ala-Houhala M, Wikström S. Risk of renal scarring in vesicoureteral reflux detected either antenatally or during the neonatal period. Urology 2003; 61 (6): 1242–1243. DOI: 10.1016/s0090-4295(03)00229-2.
- Rolleston GL, Shannon FT, Utley WL. Relationship of infantile vesicoureteric reflux to renal damage. Br Med J 1970; 1 (5694): 460–463. DOI: 10.1136/bmj.1.5694.460.
- Duckett JW, Walker RD, Weiss R. Surgical results: International Reflux Study in Children\–United States branch. J Urol 1992. DOI: 10.1016/s0022-5347(17)36999-9.
- Berg UB. Long-term followup of renal morphology and function in children with recurrent pyelonephritis. J Urol 1992. DOI: 10.1016/s0022-5347(17)37012-x.
- Nepple KG, Knudson MJ, Austin JC. Abnormal renal scans and decreased early resolution of low grade vesicoureteral reflux. Suppl):1643-7; Discussion 1647 2008; 180(4. DOI: 10.1016/j.juro.2008.03.102.
- Metcalfe CB, Macneily AE, Afshar K. Reliability assessment of international grading system for vesicoureteral reflux. J Urol 2012; 188(4. DOI: 10.1016/j.juro.2012.02.015.
- Greenfield SP, Carpenter MA, Chesney RW. The RIVUR voiding cystourethrogram pilot study: experience with radiologic reading concordance. J Urol 2012; 188(4. DOI: 10.1016/j.juro.2012.06.032.
- Cooper CS, Alexander SE, Kieran K. Utility of the distal ureteral diameter on VCUG for grading VUR. J Pediatr Urol 2015; 11 (4). DOI: 10.1016/j.jpurol.2015.04.009.
- Arlen AM, Leong T, Guidos PJ. Distal Ureteral Diameter Ratio is Predictive of Breakthrough Febrile Urinary Tract Infection. J Urol 2017; 198 (6): 1418–1423. DOI: 10.1016/j.juro.2017.06.095.
- Cooper CS, Birusingh KK, Austin JC. Distal ureteral diameter measurement objectively predicts vesicoureteral reflux outcome. J Pediatr Urol 2013; 9 (1): 99–103. DOI: 10.1016/j.jpurol.2011.12.011.
- Arlen AM, Kirsch AJ, Leong T. Validation of the ureteral diameter ratio for predicting early spontaneous resolution of primary vesicoureteral reflux. J Pediatr Urol 2017; 13 (4). DOI: 10.1016/j.jpurol.2017.01.012.
- Troesch VL, Wald M, Bonnett MA. The additive impact of the distal ureteral diameter ratio in predicting early breakthrough urinary tract infections in children with vesicoureteral reflux. J Pediatr Urol 2021; 17 (2). DOI: 10.1016/j.jpurol.2021.01.003.
- Alexander SE, Arlen AM, Storm DW. Bladder volume at onset of vesicoureteral reflux is an independent risk factor for breakthrough febrile urinary tract infection. J Urol 2015; 193 (4): 1342–1346. DOI: 10.1016/j.juro.2014.10.002.
- McMillan ZM, Austin JC, Knudson MJ. Bladder volume at onset of reflux on initial cystogram predicts spontaneous resolution. J Urol 2006. DOI: 10.1016/s0022-5347(06)00619-7.
- Nepple KG, Knudson MJ, Austin JC. Adding renal scan data improves the accuracy of a computational model to predict vesicoureteral reflux resolution. Suppl):1648-52; Discussion 1652 DOI: 101016/Jjuro200803109 PMID 2008; 180(4: 1648–1652. DOI: 10.1016/j.juro.2008.03.109.
- Knudson MJ, Austin JC, Wald M. Computational model for predicting the chance of early resolution in children with vesicoureteral reflux. Pt 2):1824-7 DOI: 101016/Jjuro200705093 PMID 2007; 178: 1824–1827. DOI: 10.1016/j.juro.2007.05.093.
- Knudson MJ, Austin JC, McMillan ZM. Predictive factors of early spontaneous resolution in children with primary vesicoureteral reflux. J Urol 2007; 178(4. DOI: 10.1016/j.juro.2007.03.161.
- KJ A, MT M, JC A. Nuclear cystometrogram-determined bladder pressure at onset of vesicoureteral reflux predicts spontaneous resolution. Urology 2007; 69 (4): 767–770. DOI: 10.1016/j.urology.2007.01.048.
- Cooper CS, Madsen MT, Austin JC. Bladder pressure at the onset of vesicoureteral reflux determined by nuclear cystometrogram. J Urol 2003; 170: 1537–1540. DOI: 10.1097/01.ju.0000083638.36182.5e.
- Arsanjani A, Alagiri M. Identification of filling versus voiding reflux as predictor of clinical outcome. Urology 2007; 70 (2): 351–354. DOI: 10.1016/j.urology.2007.03.031.
- Garcia-Roig M, Ridley DE, McCracken C. Vesicoureteral Reflux Index: Predicting Primary Vesicoureteral Reflux Resolution in Children Diagnosed after Age 24 Months. J Urol 2017; 197 (4): 1150–1157. DOI: 10.1016/j.juro.2016.12.008.
- Arlen AM, Leong T, Wu CQ. Predicting Breakthrough Urinary Tract Infection: Comparative Analysis of Vesicoureteral Reflux Index, Reflux Grade and Ureteral Diameter Ratio. J Urol 2020; 204 (3): 572–577. DOI: 10.1097/JU.0000000000001035.
- Keren R, Shaikh N, Pohl H. Risk Factors for Recurrent Urinary Tract Infection and Renal Scarring. Pediatrics 2015; 136 (1). DOI: 10.1542/peds.2015-0409.
- Lenaghan D, Whitaker JG, Jensen F. The natural history of reflux and long-term effects of reflux on the kidney. J Urol 1976; 115 (6): 10 1016 0022–5347 17 59352–59350. DOI: 10.1016/s0022-5347(17)59352-0.
- Olbing H, Claësson I, Ebel KD. Renal scars and parenchymal thinning in children with vesicoureteral reflux: a 5-year report of the International Reflux Study in Children (European branch. J Urol 1992. DOI: 10.1016/s0022-5347(17)36995-1.
- Mingin GC, Nguyen HT, Baskin LS. Abnormal dimercapto-succinic acid scans predict an increased risk of breakthrough infection in children with vesicoureteral reflux. J Urol 2004; 172 (3): 1075–1077. DOI: 10.1097/01.ju.0000135750.17348.e4.
- Loukogeorgakis SP, Burnand K, MacDonald A. Renal scarring is the most significant predictor of breakthrough febrile urinary tract infection in patients with simplex and duplex primary vesico-ureteral reflux. J Pediatr Urol 2020; 16 (2). DOI: 10.1016/j.jpurol.2019.11.018.
- Wallace DM, Rothwell DL, Williams DI. The long-term follow-up of surgically treated vesicoureteric reflux. Br J Urol 1978; 50 (7): 10 1111 1464–1410 1978 06195. DOI: 10.1111/j.1464-410x.1978.tb06195.x.
- Edwards D, Normand IC, Prescod N. Disappearance of vesicoureteric reflux during long-term prophylaxis of urinary tract infection in children. Br Med J 1977; 2 (6082): 285–288. DOI: 10.1136/bmj.2.6082.285.
- Jodal U, Lindberg U. Guidelines for management of children with urinary tract infection and vesico-ureteric reflux. Recommendations from a Swedish state-of-the-art conference. Swedish Medical Research Council Acta Paediatr Suppl 1999; 88 (431): 87–89. DOI: 10.1111/j.1651-2227.1999.tb01323.x.
- Mor Y, Leibovitch I, Zalts R. Analysis of the long-term outcome of surgically corrected vesico-ureteric reflux. BJU Int 2003; 92 (1): 10 1046 1464–1410 2003 04264. DOI: 10.1046/j.1464-410x.2003.04264.x.
- Lebowitz RL. The detection and characterization of vesicoureteral reflux in the child. J Urol 1992. DOI: 10.1016/s0022-5347(17)36991-4.
- Dalirani R, Mahyar A, Sharifian M. The value of direct radionuclide cystography in the detection of vesicoureteral reflux in children with normal voiding cystourethrography. Pediatr Nephrol 2014; 29 (12): 10 1007 00467–00014–2871–. DOI: 10.1007/s00467-014-2871-y.
- McLaren CJ, Simpson ET. Direct comparison of radiology and nuclear medicine cystograms in young infants with vesico-ureteric reflux. BJU Int 2001; 87 (1): 10 1046 1464–1410 2001 00997. DOI: 10.1046/j.1464-410x.2001.00997.x.
- Frimberger D, Mercado-Deane MG, McKenna PH. Establishing a Standard Protocol for the Voiding Cystourethrography. Pediatrics 2016; 138 (5): 10 1542 2016–2590. DOI: 10.1542/9781610021494-part05-establishing_a_stand.
- Strauss KJ, Kaste SC. The ALARA (as low as reasonably achievable) concept in pediatric interventional and fluoroscopic imaging: striving to keep radiation doses as low as possible during fluoroscopy of pediatric patients\–a white paper executive summary. Radiology 2006; 240 (3): 621–622. DOI: 10.1148/radiol.2403060698.
- Arant BS Jr. Vesicoureteral reflux and evidence-based management. J Pediatr 2001; 139 (5): 620–621. DOI: 10.1067/mpd.2001.119451.
- Shiraishi K, Matsuyama H, Nepple KG. Validation of a prognostic calculator for prediction of early vesicoureteral reflux resolution in children. J Urol 2009; 182 (2): 690–691. DOI: 10.1016/j.juro.2009.04.036.
- Kim D, Choi YH, Choi G. Contrast-enhanced voiding urosonography for the diagnosis of vesicoureteral reflux and intrarenal reflux: a comparison of diagnostic performance with fluoroscopic voiding cystourethrography. Ultrasonography 2021; 40 (4): 530–537. DOI: 10.14366/usg.20157.
- Ntoulia A, Back SJ, Shellikeri S. Contrast-enhanced voiding urosonography (ceVUS) with the intravesical administration of the ultrasound contrast agent OptisonTM for vesicoureteral reflux detection in children: a prospective clinical trial. Pediatr Radiol 2018; 48 (2): 10 1007 00247–00017–4026–4023. DOI: 10.1007/s00247-017-4026-3.
- Elison BS, Taylor D, Wall H. Comparison of DMSA scintigraphy with intravenous urography for the detection of renal scarring and its correlation with vesicoureteric reflux. Br J Urol 1992; 69 (3): 10 1111 1464–1410 1992 15532. DOI: 10.1111/j.1464-410x.1992.tb15532.x.
- Majd M, Nussbaum Blask AR, Markle BM. Acute pyelonephritis: comparison of diagnosis with 99mTc-DMSA, SPECT, spiral CT, MR imaging, and power Doppler US in an experimental pig model. Radiology 2001; 218 (1): 101–108. DOI: 10.1148/radiology.218.1.r01ja37101.
- Hamoui N, Hagerty JA, Maizels M. Ultrasound fails to delineate significant renal pathology in children with urinary tract infections: a case for dimercapto-succinic acid scintigraphy. Suppl):1639-42; Discussion 1642 2008; 180(4. DOI: 10.1016/j.juro.2008.03.119.
- Smokvina A, Grbac-Ivanković S, Girotto N. The renal parenchyma evaluation: MAG3 vs. DMSA Coll Antropol 2005; 29 (2): 649–654.
- Sfakianakis GN, Cavagnaro F, Zilleruelo G. Diuretic MAG3 scintigraphy (F0) in acute pyelonephritis: regional parenchymal dysfunction and comparison with DMSA. J Nucl Med 2000; 41 (12): 1955–1963.
- Gordon I, Anderson PJ, Lythgoe MF. Can technetium-99m-mercaptoacetyltriglycine replace technetium-99m-dimercaptosuccinic acid in the exclusion of a focal renal defect? J Nucl Med 1992; 33 (12): 1334134.
- Lee RS, Cendron M, Kinnamon DD. Antenatal hydronephrosis as a predictor of postnatal outcome: a meta-analysis. Pediatrics 2006; 118 (2): 586–593. DOI: 10.1542/PEDS.2006-0120.
- Herndon CDA, McKenna PH, Kolon TF. A multicenter outcomes analysis of patients with neonatal reflux presenting with prenatal hydronephrosis. J Urol 1999; 162 (3 Pt 2): 1203–1208. DOI: 10.1097/00005392-199909000-00096.
- Nguyen HT, Herndon CDA, Cooper C. The Society for Fetal Urology consensus statement on the evaluation and management of antenatal hydronephrosis. J Pediatr Urol 2010; 6 (3): 212–231. DOI: 10.1016/J.JPUROL.2010.02.205.
- Upadhyay J, McLorie GA, Bolduc S. Natural history of neonatal reflux associated with prenatal hydronephrosis: Long-term results of a prospective study. J Urol 2003; 169 (5): 1837–1841. DOI: 10.1097/01.ju.0000062440.92454.cf.
- Berrocal T, Pinilla I, Gutiérrez J. Mild hydronephrosis in newborns and infants: can ultrasound predict the presence of vesicoureteral reflux. Pediatr Nephrol 2007; 22 (1): 91–96. DOI: 10.1007/S00467-006-0285-1.
- Farhat W, McLorie G, Geary D. The natural history of neonatal vesicoureteral reflux associated with antenatal hydronephrosis. J Urol 2000; 164 (3 Pt 2): 1057–1060. DOI: 10.1097/00005392-200009020-00033.
- M A, K W-L, BK V. Society for fetal urology recommendations for postnatal evaluation of prenatal hydronephrosis\–will fewer voiding cystourethrograms lead to more urinary tract infections? J Urol 2013. DOI: 10.1016/J.JURO.2013.03.038.
- Braga LH, Farrokhyar F, DĆruz J. Risk factors for febrile urinary tract infection in children with prenatal hydronephrosis: a prospective study. J Urol 2015. DOI: 10.1016/J.JURO.2014.10.091.
- Zee RS, Herndon CDA, Cooper CS. Time to resolution: A prospective evaluation from the Society for Fetal Urology hydronephrosis registry. J Pediatr Urol 2017; 13 (3). DOI: 10.1016/J.JPUROL.2016.12.012.
- Silay MS, Undre S, Nambiar AK. Role of antibiotic prophylaxis in antenatal hydronephrosis: A systematic review from the European Association of Urology/European Society for Paediatric Urology Guidelines Panel. J Pediatr Urol 2017; 13 (3): 306–315. DOI: 10.1016/J.JPUROL.2017.02.023.
- Braga LH, Mijovic H, Farrokhyar F. Antibiotic prophylaxis for urinary tract infections in antenatal hydronephrosis. Pediatrics 2013; 131 (1): 10 1542 2012–1870. DOI: 10.1542/peds.2012-1870.
- Easterbrook B, Capolicchio JP, Braga LH. Antibiotic prophylaxis for prevention of urinary tract infections in prenatal hydronephrosis: An updated systematic review. Can Urol Assoc J 2017; 11 (1-2Suppl1). DOI: 10.5489/CUAJ.4384.
- Zareba P, Lorenzo AJ, Braga LH. Risk factors for febrile urinary tract infection in infants with prenatal hydronephrosis: comprehensive single center analysis. J Urol 2014. DOI: 10.1016/J.JURO.2013.10.035.
- Coelho GM, Bouzada MCF, Pereira AK. Outcome of isolated antenatal hydronephrosis: a prospective cohort study. Pediatr Nephrology 2007; 22 (10): 1727–1734. DOI: 10.1007/S00467-007-0539-6.
- Szymanski KM, Al-Said AN, Pippi Salle JL. Do infants with mild prenatal hydronephrosis benefit from screening for vesicoureteral reflux? J Urol 2012; 188 (2): 576–581. DOI: 10.1016/J.JURO.2012.04.017.
- Routh JC, Grant FD, Kokorowski P. Costs and consequences of universal sibling screening for vesicoureteral reflux: decision analysis. Pediatrics 2010; 126 (5): 10 1542 2010–0744. DOI: 10.1542/peds.2010-0744d.
- Hunziker M, Colhoun E, Puri P. Renal cortical abnormalities in siblings of index patients with vesicoureteral reflux. Pediatrics 2014; 133 (4): 10 1542 2013–3498. DOI: 10.1542/peds.2013-3498d.
- Nelson CP, Finkelstein JA, Logvinenko T. Incidence of Urinary Tract Infection Among Siblings of Children With Vesicoureteral Reflux. Acad Pediatr 2016; 16 (5): 489–495. DOI: 10.1016/j.acap.2015.11.003.
- Skoog SJ, Peters CA, Arant BS Jr.. Pediatric Vesicoureteral Reflux Guidelines Panel Summary Report: Clinical Practice Guidelines for Screening Siblings of Children With Vesicoureteral Reflux and Neonates/Infants With Prenatal Hydronephrosis. J Urol 2010; 184 (3): 1145–1151. DOI: 10.1016/j.juro.2010.05.066.
- Urinary Tract Infection SCoQI S, Management RKB. Urinary Tract Infection: Clinical Practice Guideline for the Diagnosis and Management of the Initial UTI in Febrile Infants and Children 2 to 24 Months. Pediatrics 2011; 128 (3): 595–610. DOI: 10.1542/peds.2011-1330.
- Mattoo TK, Carpenter MA, Moxey-Mims M. The RIVUR trial: a factual interpretation of our data. Pediatr Nephrol 2015; 30 (5): 10 1007 00467–00014–3022–3021. DOI: 10.1007/s00467-014-3022-1.
- Shaikh N, Haralam MA, Kurs-Lasky M. Association of Renal Scarring With Number of Febrile Urinary Tract Infections in Children. JAMA Pediatrics 2019; 173 (10): 949–952. DOI: 10.1001/JAMAPediatrics.2019.2504.
- Coulthard MG, Flecknell P, Orr H. Renal scarring caused by vesicoureteric reflux and urinary infection: a study in pigs. Pediatr Nephrol 2002; 17 (7): 10 1007 00467–00002–0878–0872. DOI: 10.1007/s00467-002-0878-2.
- Montini G, Rigon L, Zucchetta P. Prophylaxis after first febrile urinary tract infection in children? A multicenter, randomized, controlled, noninferiority trial. Pediatrics 2008; 122 (5): 1064–1071. DOI: 10.1542/peds.2007-3770.
- Pennesi M, Travan L, Peratoner L. Is antibiotic prophylaxis in children with vesicoureteral reflux effective in preventing pyelonephritis and renal scars? A randomized, controlled trial. Pediatrics 2008; 121 (6): 10 1542 2007–2652. DOI: 10.1542/peds.2008-2339.
- Roussey-Kesler G, Gadjos V, Idres N. Antibiotic prophylaxis for the prevention of recurrent urinary tract infection in children with low grade vesicoureteral reflux: Results from a prospective randomized study. J Urol 2008; 179 (2): 674–679. DOI: 10.1016/J.JURO.2007.09.090.
- Conway PH, Cnaan A, Zaoutis T. Recurrent urinary tract infections in children: risk factors and association with prophylactic antimicrobials. JAMA 2007; 298 (2): 179–186. DOI: 10.1001/jama.298.2.179.
- Investigators RT, Hoberman A, Greenfield SP. Antimicrobial Prophylaxis for Children with Vesicoureteral Reflux. New Engl J Med 2014; 370 (25): 2367–2376. DOI: 10.1056/NEJMoa1401811.
- Cooper CS, Chung BI, Kirsch AJ. The outcome of stopping prophylactic antibiotics in older children with vesicoureteral reflux. J Urol 2000; 163 (1): 269–273. DOI: 10.1016/S0022-5347(05)68034-2.
- Thompson RH, Chen JJ, Pugach J. Cessation of prophylactic antibiotics for managing persistent vesicoureteral reflux. J Urol 2001; 166 (4): 1465–1469. DOI: 10.1097/00005392-200110000-00072.
- Jodal U, Koskimies O, Hanson E. Infection pattern in children with vesicoureteral reflux randomly allocated to operation or long-term antibacterial prophylaxis. The International Reflux Study in Children. J Urol 1992. DOI: 10.1016/s0022-5347(17)36994-x.
- Bailey RR. Commentary: the management of grades I and II (nondilating) vesicoureteral reflux. J Urol 1992. DOI: 10.1016/s0022-5347(17)37004-0.
- A prospective trial of operative versus non-operative treatment of severe vesico-ureteric reflux: 2 years\’observation in 96 children. The Birmingham Reflux Study Group. Contrib Nephrol 1984; 39 (169-85): 6744870. DOI: 10.1136/bmj.295.6592.237.
- Leslie B, Moore K, Salle JL. Outcome of antibiotic prophylaxis discontinuation in patients with persistent vesicoureteral reflux initially presenting with febrile urinary tract infection: time to event analysis. J Urol 2010; 184 (3): 1093–1098. DOI: 10.1016/j.juro.2010.05.013.
- Allen UD, MacDonald N, Fuite L. Risk factors for resistance to f́irst-line\’antimicrobials among urinary tract isolates of Escherichia coli in children. CMAJ 1999; 160 (10): 1436–1440.
- Cheng CH, Tsai MH, Huang YC. Antibiotic Resistance Patterns of Community-Acquired Urinary Tract Infections in Children With Vesicoureteral Reflux Receiving Prophylactic Antibiotic Therapy. Pediatrics 2008; 122 (6): 1212–1217. DOI: 10.1542/peds.2007-2926.
- Cooper CS. Fat, demented and stupid: An unrecognized legacy of pediatric urology? J Pediatr Urol 2017; 13 (4): 341–344. DOI: 10.1016/J.JPUROL.2017.04.027.
- Guidos PJ, Arlen AM, Leong T. Impact of continuous low-dose antibiotic prophylaxis on growth in children with vesicoureteral reflux. J Pediatr Urol 2018; 14 (4). DOI: 10.1016/J.JPUROL.2018.07.007.
- Gaither TW, Cooper CS, Kornberg Z. Predictors of becoming overweight among pediatric patients at risk for urinary tract infections. J Pediatr Urol 2019; 15 (1). DOI: 10.1016/J.JPUROL.2018.09.002.
- Akagawa Y, Kimata T, Akagawa S. Impact of Long-Term Low Dose Antibiotic Prophylaxis on Gut Microbiota in Children. J Urol 2020; 204 (6): 1320–1325. DOI: 10.1097/JU.0000000000001227.
- Copp HL, Nelson CP, Shortliffe LD. Compliance with antibiotic prophylaxis in children with vesicoureteral reflux: results from a national pharmacy claims database. J Urol 2010; 183 (5): 1994–2000. DOI: 10.1016/J.JURO.2010.01.036.
- Fast AM, Nees SN, Batavia JP. Outcomes of targeted treatment for vesicoureteral reflux in children with nonneurogenic lower urinary tract dysfunction. J Urol 2013; 190 (3): 1028–1032. DOI: 10.1016/j.juro.2013.03.005.
- Smellie JM. Commentary: management of children with severe vesicoureteral reflux. J Urol 1992. DOI: 10.1016/s0022-5347(17)37000-3.
- J BM, editor. Prospective trial of operative versus non-operative treatment of severe vesicoureteric reflux in children: five years\’observation. Birmingham Reflux Study Group. 1987; 295 (6592): 237–241. DOI: 10.1136/bmj.295.6592.237.
- Elo J, Tallgren LG, Alfthan O. Character of urinary tract infections and pyelonephritic renal scarring after antireflux surgery. J Urol 1983; 129 (2): 6834504. DOI: 10.1016/s0022-5347(17)52089-3.
- Belman AB. Vesicoureteral reflux. Pediatr Clin North Am 1997; 44 (5): 9326957. DOI: 10.53347/rid-12076.
- Ransley PG, Risdon RA. The pathogenesis of reflux nephropathy. Contrib Nephrol 1979; 16: 90–97. DOI: 10.1159/000402880.
- Molitierno JA, Scherz HC, Kirsch AJ. Endoscopic treatment of vesicoureteral reflux using dextranomer hyaluronic acid copolymer. J Pediatr Urol 2008; 4 (3): 221–228. DOI: 10.1016/j.jpurol.2007.11.015.
- Stenberg AM, Sundin A, Larsson BS. Lack of distant migration after injection of a 125iodine labeled dextranomer based implant into the rabbit bladder. J Urol 1997; 158 (5): 10 1016 0022–5347 01 64185–64185. DOI: 10.1016/s0022-5347(01)64185-5.
- Läckgren G, Wåhlin N, Sköldenberg E. Long-term followup of children treated with dextranomer/hyaluronic acid copolymer for vesicoureteral reflux. J Urol 2001; 166 (5): 10 1016 0022–5347 05 65713–65718. DOI: 10.1097/00005392-200111000-00076.
- Kirsch AJ, Perez-Brayfield MR, Scherz HC. Minimally invasive treatment of vesicoureteral reflux with endoscopic injection of dextranomer/hyaluronic acid copolymer: the Childrenś Hospitals of Atlanta experience. J Urol 2003; 170 (1): 211–215. DOI: 10.1097/01.ju.0000072523.43060.a0.
- Dave S, Lorenzo AJ, Khoury AE. Learning from the learning curve: factors associated with successful endoscopic correction of vesicoureteral reflux using dextranomer/hyaluronic acid copolymer. J Urol 2008; 180(4: 1594–1599. DOI: 10.1016/j.juro.2008.03.084.
- Kirsch AJ, Perez-Brayfield M, Smith EA. The modified sting procedure to correct vesicoureteral reflux: improved results with submucosal implantation within the intramural ureter. J Urol 2004; 171 (6 Pt 1): 2413–2416. DOI: 10.1097/01.ju.0000127754.79866.7f.
- McMann LP, Scherz HC, Kirsch AJ. Long-term preservation of dextranomer/hyaluronic acid copolymer implants after endoscopic treatment of vesicoureteral reflux in children: a sonographic volumetric analysis. J Urol 2007; 177 (1): 320. DOI: 10.1016/j.juro.2006.08.144.
- Baydilli N, Selvi I, Pinarbasi AS. Additional VCUG-related parameters for predicting the success of endoscopic injection in children with primary vesicoureteral reflux. J Pediatr Urol 2021; 17 (1). DOI: 10.1016/j.jpurol.2020.11.018.
- Kirsch AJ, Cooper CS, Läckgren G. Non-Animal Stabilized Hyaluronic Acid/Dextranomer Gel (NASHA/Dx, Deflux) for Endoscopic Treatment of Vesicoureteral Reflux: What Have We Learned Over the Last 20 Years? Urology 2021; 157: 15–28. DOI: 10.1016/j.urology.2021.07.032.
- Routh JC, Inman BA, Reinberg Y. Dextranomer/hyaluronic acid for pediatric vesicoureteral reflux: systematic review. Pediatrics 2010; 125 (5): 10 1542 2009–2225. DOI: 10.1016/j.yped.2011.04.057.
- Elder JS, Diaz M, Caldamone AA. Endoscopic therapy for vesicoureteral reflux: a meta-analysis. I. Reflux resolution and urinary tract infection. J Urol 2006; 175 (2): 10 1016 0022–5347 05 00210–00217. DOI: 10.1016/s0084-4071(08)70406-8.
- Arlen AM, Scherz HC, Filimon E. Is routine voiding cystourethrogram necessary following double hit for primary vesicoureteral reflux? J Pediatr Urol 2015; 11 (1). DOI: 10.1016/j.jpurol.2014.11.011.
- Wang PZT, Abdelhalim A, Walia A. Avoiding routine postoperative voiding cystourethrogram: Predicting radiologic success for endoscopically treated vesicoureteral reflux. Can Urol Assoc J 2019; 13 (5). DOI: 10.5489/cuaj.5589.
- Knudson MJ, Cooper CS, Block CA. Calcification of glutaraldehyde cross-linked collagen in bladder neck injections in children with incontinence: a long-term complication. J Urol 2006; 176 (3): 1143–1146. DOI: 10.1016/j.juro.2006.04.059.
- Gargollo PC, Paltiel HJ, Rosoklija I. Mound calcification after endoscopic treatment of vesicoureteral reflux with autologous chondrocytes\–a normal variant of mound appearance? J Urol 2009; 181 (6): 2707–2708. DOI: 10.1016/j.juro.2009.02.053.
- Noe HN. Calcification in a Deflux bleb thought to be a ureteral calculus in a child. J Pediatr Urol 2008; 4 (1): 88–89. DOI: 10.1016/j.jpurol.2007.02.005.
- Vandersteen DR, Routh JC, Kirsch AJ. Postoperative ureteral obstruction after subureteral injection of dextranomer/hyaluronic Acid copolymer. J Urol 2006; 176(4. DOI: 10.1016/j.juro.2006.06.101.
- Papagiannopoulos D, Rosoklija I, Cheng E. Delayed Obstruction With Asymptomatic Loss of Renal Function After Dextranomer/Hyaluronic Acid Copolymer (Deflux) Injection for Vesicoureteral Reflux: A Close Look at a Disturbing Outcome. Urology 2017; 101: 63–66. DOI: 10.1016/j.urology.2016.09.013.
- Romain J, Fourcade L, Centi J. Delayed-onset Ureteral Obstruction and Calcification Masquerading as Renal Colic Following Deflux Injection. Urology 2016; 94: 218–220. DOI: 10.1016/j.urology.2016.03.001.
- Christen S, Mendoza M, Gobet R. Late ureteral obstruction after injection of dextranomer/hyaluronic acid copolymer. Urology 2014; 83 (4): 920–922. DOI: 10.1016/j.urology.2013.10.053.
- Austin JC, Cooper CS. Vesicoureteral reflux: surgical approaches. Urol Clin North Am 2004; 31 (3): 543–557. DOI: 10.1016/j.ucl.2004.04.018.
- Sprunger JK, Reese CT, Decter RM. Can standard open pediatric urological procedures be performed on an outpatient basis? J Urol 2001; 166 (3): 1062–1064. DOI: 10.1097/00005392-200109000-00083.
- Marotte JB, Smith DP. Extravesical ureteral reimplantations for the correction of primary reflux can be done as outpatient procedures. J Urol 2001; 165 (6 Pt 2): 10 1097 00005392–200106001–00003. DOI: 10.1016/s0022-5347(05)66171-x.
- Palmer JS. Bilateral extravesical ureteral reimplantation in toilet-trained children: short-stay procedure without urinary retention. Urology 2009; 73 (2): 285–288. DOI: 10.1016/j.urology.2008.07.046.
- Barrieras D, Lapointe S, Reddy PP. Are postoperative studies justified after extravescial ureteral reimplantation? J Urol 2000; 164(3. DOI: 10.1097/00005392-200009020-00035.
- Bisignani G, Decter RM. Voiding cystourethrography after uncomplicated ureteral reimplantation in children: is it necessary? J Urol 1997; 158(3. DOI: 10.1016/s0022-5347(01)64437-9.
- El-Ghoneimi A, Odet E, Lamer S. Cystography after the Cohen ureterovesical reimplantation: is it necessary at a training center? J Urol 1999; 162(3. DOI: 10.1016/s0022-5347(01)68133-3.
- Harel M, Herbst KW, Silvis R. Objective pain assessment after ureteral reimplantation: comparison of open versus robotic approach. J Pediatr Urol 2015; 11 (2). DOI: 10.1016/j.jpurol.2014.12.007.
- Boysen WR, Ellison JS, Kim C. Multi-Institutional Review of Outcomes and Complications of Robot-Assisted Laparoscopic Extravesical Ureteral Reimplantation for Treatment of Primary Vesicoureteral Reflux in Children. J Urol 2017; 197 (6): 1555–1561. DOI: 10.1016/j.juro.2017.01.062.
- Kurtz MP, Leow JJ, Varda BK. Robotic versus open pediatric ureteral reimplantation: Costs and complications from a nationwide sample. J Pediatr Urol 2016; 12 (6). DOI: 10.1016/j.jpurol.2016.06.016.
- Bowen DK, Faasse MA, Liu DB. Use of Pediatric Open, Laparoscopic and Robot-Assisted Laparoscopic Ureteral Reimplantation in the United States: 2000 to 2012. J Urol 2016; 196 (1): 207–212. DOI: 10.1016/j.juro.2016.02.065.
- Rolleston GL, Maling TM, Hodson CJ. Intrarenal reflux and the scarred kidney. Arch Dis Child 1974; 49 (7): 531–539. DOI: 10.1136/adc.49.7.531.
- Austin JC. Treatment of vesicoureteral reflux after puberty. Adv Urol 2008; 2008 (590185). DOI: 10.1155/2008/590185.
最近更新时间: 2025-09-22 08:00